Chronic suppurative lacrimal canaliculitis is an important cause of ocular surface discomfort. Being a relatively rare condition, it is commonly overlooked and undiagnosed for long periods of time. Actinomyces israelii is classically cited as the most common causative organism of canaliculitis,1 at the same time, isolation is difficult owing to the anaerobic nature of the pathogen. Herein we present a case of chronic lacrimal canaliculitis successfully managed with the therapeutic triad of surgery, systemic antibiotics, and topical eye drops to increase awareness for this treatable condition.
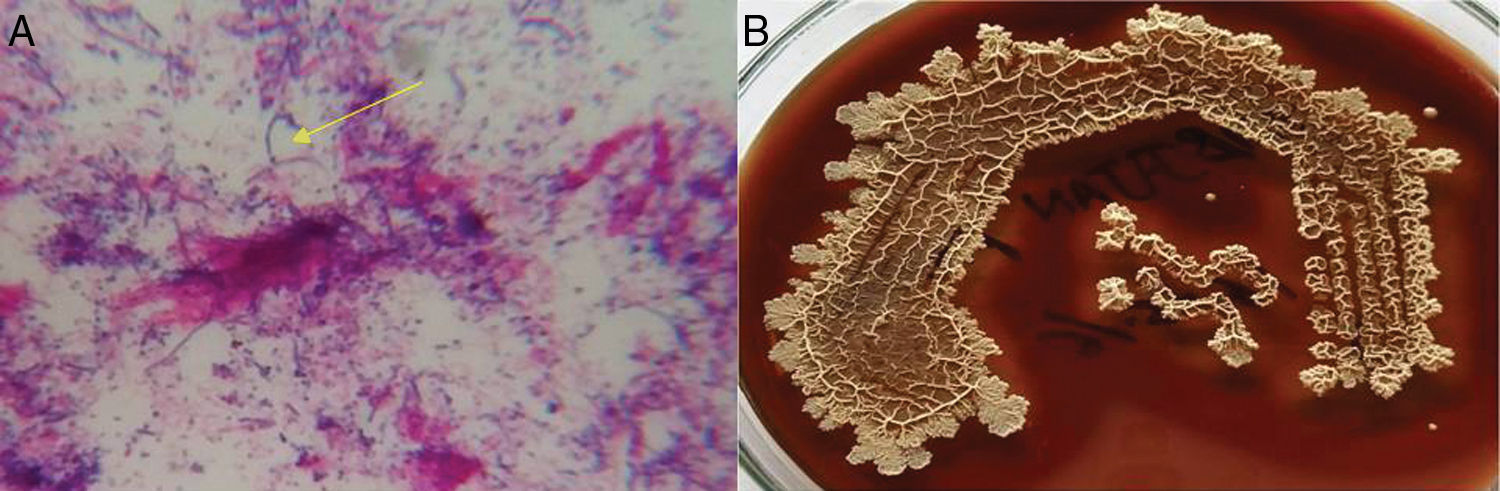
A 75-year-old male, retired personnel, presented with complaints of swelling at medial canthus of the left eye of one-year duration associated with pain, ocular discharge, redness, and watering. Prior to his visit at our hospital, he had consulted another hospital and received certain medications for his symptoms, but without relief. He was a known diabetic since 10 years, on oral glucose lowering agents and had primary open angle glaucoma. There was no history of trauma, or ocular surgery within the past six months. Ocular examination revealed swelling near left punctum associated with pouting of punctum with yellowish whitish material (sulfur granules) blocking the punctum. A Gram stain of the sulfur granules showed, Gram positive, non-acid fast, branching filaments, suggestive of Actinomyces species (Fig. 1A). Anaerobic culture yielded irregular, grey, non-hemolytic, molar tooth colonies of Gram-positive bacilli, negative for catalase, urease, and indole tests but positive for esculin hydrolysis test, identified as A. israelii (Fig. 1B). A therapeutic triad of one-snip punctoplasty procedure, curettage along with oral amoxillin-clavulanic acid for 10 days and topical chloramphenicol eye drops resulted in resolution. The patient had no purulent discharge or recurrence at six months follow-up.
The fact that A. israelii can cause conjunctivitis or lacrimal canaliculitis without any generalized systemic invasion is a relatively less recognized clinical phenomenon. Nevertheless, A. israelii is reported as the most common causative agent of primary lacrimal canaliculitis with a reported frequency of 13–25%.1 The anaerobic Gram positive bacilli aggregate to produce sulfur granules or large cheesy masses within the distended canal which may block the flow of tears. These actinomycotic granules composed of an internal tangle of mycelia fragments and a rosette of peripheral clubs, stabilized by a protein-polysaccharide complex, are supposed to provide a resistance mechanism to host defenses by inhibiting phagocytosis.2 The most commonly observed clinical features consist of epiphora with discharge (85–94%), pouting punctum (72–75%), conjunctivitis, eyelid matting, and punctual regurgitation of concretions under syringing (75%).3,4 Other pathogens known to cause concretions on the lacrimal canaliculus include, Candida albicans, Aspergillus niger, Fusobacterium species, and Nocardia asteroides.5 Patients usually undergo successful resolution of symptoms following surgery and topical antibiotics.3–5
Ophthalmic conditions reportedly misdiagnosed as lacrimal canaliculitis include mucocele, dacryocystitis, chalazia, blepharitis, and conjunctivitis. Our patient was also previously diagnosed and treated as a case of chronic conjunctivitis prior to his presentation at our hospital. Therefore, it is important to consider the diagnosis of lacrimal canaliculitis while seeing any of the above mentioned cases. Greater awareness of this condition would prevent misdiagnosis and delays in referral for definitive treatment.
Conflicts of interestThe authors declare no conflicts of interest.