Early initiation of antiretroviral therapy increases the likelihood of effective immune restoration, quality of life, and greater life expectancy for HIV-infected individuals. We evaluated the evolution of mean CD4+ cells count at diagnosis of HIV/AIDS in Salvador, Brazil from 2002 to 2015. We identified HIV/AIDS patients older than 18 years with diagnosis of HIV infection from 2002 to 2015, who had their first laboratory evaluation at Complexo Hospitalar Prof. Edgard Santos, Federal University of Bahia. Initial mean CD4+ cells count and age, over time were evaluated. A total of 1801 patients randomly selected individuals were included in the analysis. Overall mean CD4+ count at diagnosis in the whole period was 279±265, varying from 191 in 2015 to 334 in 2011. There was no improvement in the immunological status at diagnosis from 2002 to 2015. In addition, a higher frequency of CD4+ cells count<200cells/mL in the last two years was observed. This suggests that the adopted strategies for early diagnosis of HIV/AIDS in Salvador, Brazil, are still ineffective.
Around 38.6 million people are infected with HIV-1 worldwide. Depletion of CD4+ T cells, especially in lymphoid tissues, is the main consequence of HIV-1 infection, and leads to immunological failure in the absence of effective treatment.1
Successful antiretroviral therapy (ART) makes possible immune restoration, reducing the frequency of hospitalizations and opportunistic infections, and turning HIV/AIDS into a chronic disease. In consequence, treated HIV-infected patients may have a life expectancy similar to that observed for general population. Currently, more than 50% of the deaths in HIV-infected patients receiving effective ART are caused by non-AIDS-related problems.2
Early initiation of treatment (CD4+ cell count ≥500cells/mm3), usually provides conditions to a successful immune restoration. In addition, ART has proven to play a key role in reducing HIV transmission. Late diagnosis of HIV infection increases the risk of virus transmission and disease progression to AIDS.3–5 However, about 50% of HIV-infected-individuals worldwide do not know their status.6 In Brazil, since 2013 all HIV-infected individuals are eligible to start ART, irrespective of CD4+ cells count.7
The Brazilian Ministry of Health reported around 11,700 HIV in the study period, and the proportion of patients with a CD4+ cells count≤350cells/mm3 (“late presenters”) varied between 38% (2015) and 72% (2009).8 This study aims to evaluate the changes of mean initial CD4+ cells count for patients with a diagnosis of HIV/AIDS in Salvador, Brazil from 2002 to 2012.
We included HIV/AIDS outpatients older than 18 years who had their first laboratory evaluation at the Laboratório de Pesquisa em Infectologia (LAPI), located at Complexo Hospitalar Prof. Edgard Santos, Federal University of Bahia (CHUPES), from 2002 to 2015. The data was randomly extracted from National Database for Laboratory in HIV/AIDS (SISCEL) and electronic medical records. We collected information on the first results of CD4+ cells count and viral load for patients diagnosed in the study period. Using the official estimates for new HIV cases in the study period we selected a sample of 1801 patients (a minimum of 100patients/year) by a computer-generated list. To calculate the sample size, we used the minimal and maximal estimates for late presentation of patients in the period (40% and 72%, respectively). We added a 20% excess to account for potential problems in retrieving information. The final sample (1801 patients) provided 99.99% confidence interval.
We estimated frequencies, means, standard deviations, medians, and quartiles for the main variables using SPSS Version 20 software. Stratified analyses were performed by sex, year of diagnosis, and CD4+ cells count categories. For analysis purposes CD4+ cells count was also stratified in four distinct categories: (1) ≤200cells per mm3; (2) from 201 to 350cells per mm3; (3) from 351 to 500cells per mm3; (4) >500cells per mm3. An initial CD4+ cells count≤350cells/mm3 was considered as late presentation for health care.
A total of 1801 patients with HIV/AIDS diagnosis from 2002 to 2015 was included, 63.4% were male. Mean age at diagnosis was 37.3 years±10.3 (18.1 to 83.5 years). The mean age at diagnosis was similar overtime and oscillated from 34.4±9.4 in 2006 to 38.9±10.5 in 2013. Most (69.4%) patients lived in Salvador, 27.9% in other cities in Bahia, and 2.7% lived in other Brazilian states.
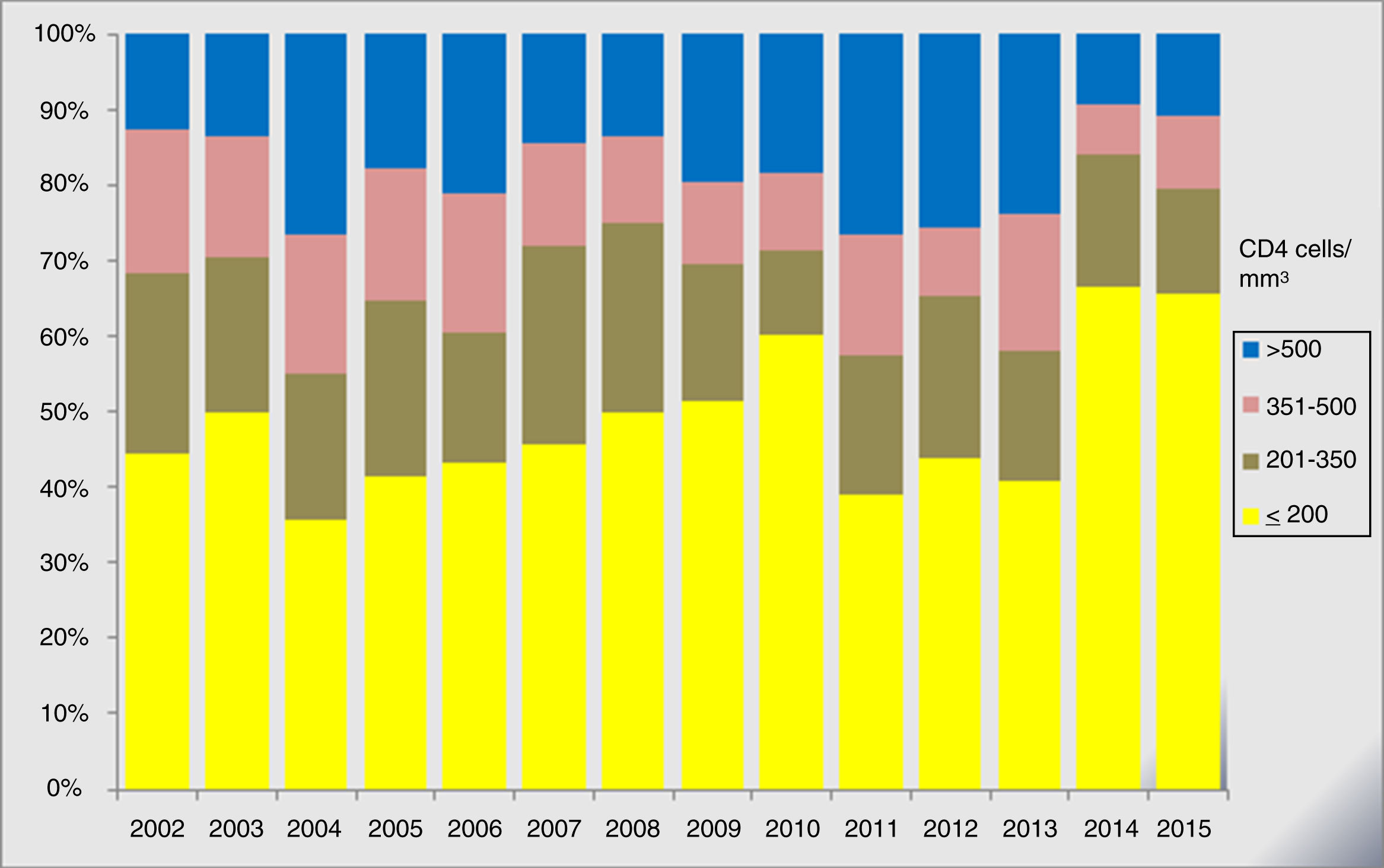
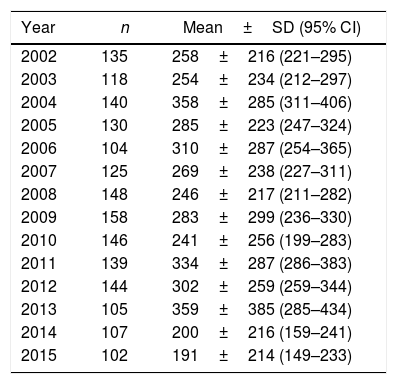
The overall CD4+ cell count mean at diagnosis in the whole period was 279±265. The plasma viral load at diagnosis oscillated from 83copies/mL to more than 500,000copies/mL while the mean CD4+ cell count ranged from 191 in 2015 to 334 in 2011. Table 1 shows the mean CD4+ cell count per year. The stratified analysis of mean CD4+ cell count showed a higher proportion of patients with a mean CD4+ cell count lower than 350cells/mm3 in the study period. It also showed a lower mean CD4+ cell count (≤200cells/mm3) in 2014 and 2015, in comparison to previous years. Fig. 1 shows the variation of mean CD4 cell count over time.
Mean CD4+ cells count (per mm3) at first medical evaluation according to the year of diagnosis.
| Year | n | Mean±SD (95% CI) |
|---|---|---|
| 2002 | 135 | 258±216 (221–295) |
| 2003 | 118 | 254±234 (212–297) |
| 2004 | 140 | 358±285 (311–406) |
| 2005 | 130 | 285±223 (247–324) |
| 2006 | 104 | 310±287 (254–365) |
| 2007 | 125 | 269±238 (227–311) |
| 2008 | 148 | 246±217 (211–282) |
| 2009 | 158 | 283±299 (236–330) |
| 2010 | 146 | 241±256 (199–283) |
| 2011 | 139 | 334±287 (286–383) |
| 2012 | 144 | 302±259 (259–344) |
| 2013 | 105 | 359±385 (285–434) |
| 2014 | 107 | 200±216 (159–241) |
| 2015 | 102 | 191±214 (149–233) |
In the present work, late presentation to health care was observed for the duration of the study, with a high proportion of patients with a CD4 count below 300cells/mm3 at first visit. In addition, the mean age at diagnosis did not present significant variation. Most individuals lived in Salvador and were expected to have easier access to health care than those living in smaller cities.
According to the Brazilian Ministry of Health, in 2015 the proportion of individuals with first CD4+ cell count lower than 200cells/mm3 had a tendency to decrease, from 31% in 2009 to 25% in 2015.8 In contrast, our results show increase in the proportion of individuals diagnosed with CD4+ cell count lower than 200cells/mm3 in the years 2014 and 2015, in Bahia. Moreover, we did not observe any improvement in the proportion of early HIV diagnosis in the last 13 years.
A similar epidemiological picture is observed in other studies. Souza-Jr et al. detected a high prevalence of HIV/AIDS diagnosis performed at an advanced stage of infection, with a consequent delay in ART introduction. Other studies carried out in Belo Horizonte, São Paulo, and Rio de Janeiro have shown that the proportion of late presentation of HIV-infected patients to health care is still high in these Brazilian states.9–12
Studies carried out in other countries have shown distinct results.6,13–17 Lesko (2013) observed that the CD4 cell count at the time of presentation for health care services had a non-significant increase in developed countries from 1992 to 2011, while Kiertiburanakul (2014) concluded that CD4 cell count at the time of ART initiation increased significantly in some Asian countries from 2007 to 2011, and that there was a significant reduction in delay to start treatment, although the late presentation rate remained elevated. The increase in frequency of early diagnosis in Asian countries was attributed to changes in health practices, updating WHO recommendations (World Health Organization) and to the expansion in availability of HIV testing during prenatal care. In addition, Ransome (2015) showed a decline in late presentation rates in New York, especially among men, which was associated to increased coverage of HIV testing from 2003 to 2010.18
Our results suggest that late-presentation is still a main problem for AIDS patients in Salvador, Brazil. We detected a concerning low mean initial CD4 cell count in the last two years. This suggests that the currently adopted strategies to increase early diagnosis of HIV/AIDS in Salvador, Brazil, are still inefficient. A wider HIV screening of people at risk and of those that present acute infection symptoms should be considered. The sample obtained from one single site is the main limitation of our work, which limits the external validity of our findings. However, LAPI performs CD4/CD8 tests and viral load for about 40% of HIV population in Bahia, which increases the overall relevance of our sample. Larger studies are necessary to confirm our results and to define the real situation of HIV diagnosis in Brazil.
Conflicts of interestThe authors declare no conflicts of interest.