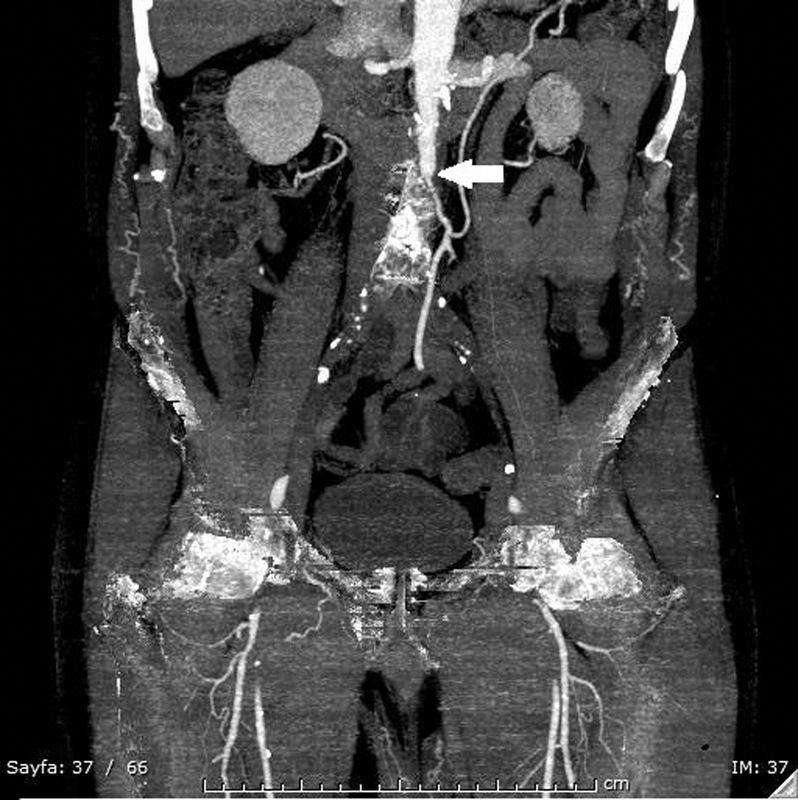
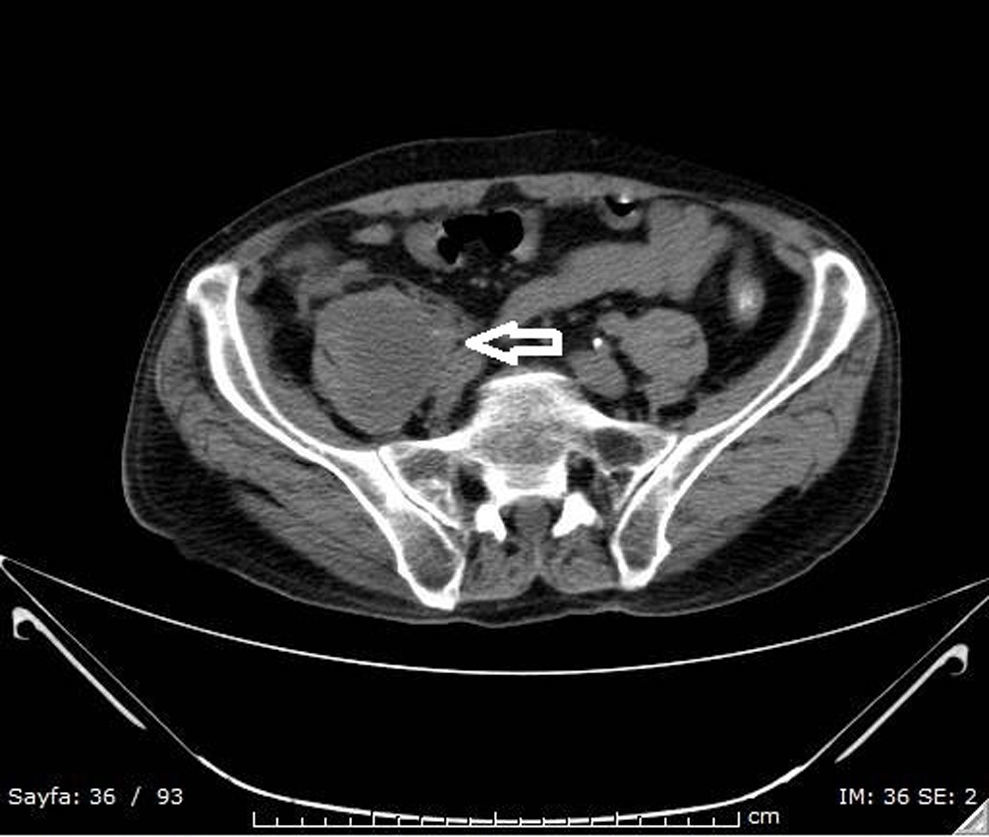
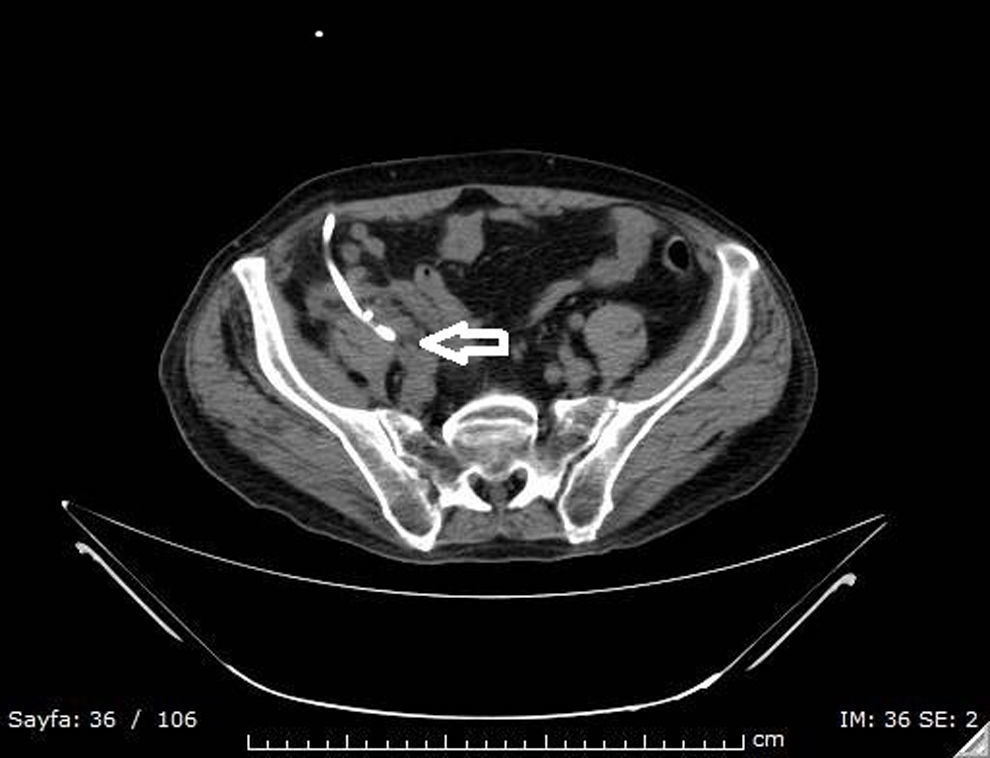
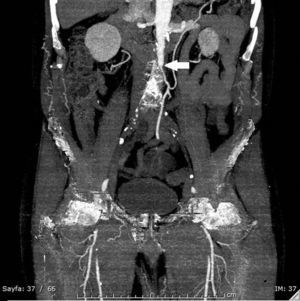
Common and applicable diagnostic methods are available for brucellosis. However, its life-threatening complications remain critical. Herein we present a 68-year-old patient who complained of leg pain for two months. At admission he had absent pulse in the left femoral and bilateral popliteal arteries. Laboratory test results were leucocytes 8700/mm3, CRP 86mg/L, and ESR 47mm/h. Abdominal CT revealed images consistent with mural thrombus in the suprarenal segment of abdominal aorta, total occlusion and hypodense thrombus material completely filling the aortic lumen through infrarenal segment extending to lumens of the caudal, bilateral common and superior iliac arteries (Figs. 1–3). No paleness, coldness or color change was detected in the lower extremities. The patient had fever, right inguinal swelling, and sweating. Abdominal CT showed an aortic thrombus and a hypodense lesion of 58mm×61mm×100mm in the right psoas muscle. The repeated Brucella STA test was positive in 1:5120 titer. USG-guided drainage of the psoas abscess was performed and a treatment with doxycycline and rifampicin was administered for three months (Fig. 4). The patient was not operated on and progressed with no clinical complaints.
Brucellosis cases with aortic occlusions and thrombus have been very rarely reported in the literature. This complication is mostly fatal in acute cases. This complication should be kept in mind especially for the patients complaining of lower extremity pain. Such pain may result from impaired circulation due to aortic thrombus, as well as from sacroiliitis and spondylodiscitis. The treatment approach for these patients in whom chronic thrombus developed without any symptom is not yet clear.1–3
Conflicts of interestThe authors declare no conflicts of interest.