To determine the appropriateness of the acute otitis media antibiotic treatment prescribed in the community in relation to the therapeutic guidelines.
MethodsChildren aged 3 months–3 years diagnosed with simple uncomplicated acute otitis media in 6 community primary care clinics were enrolled. Data on the antibiotic treatment were collected using computerized medical files.
Results689 simple uncomplicated acute otitis media patients were enrolled; 597 (86.9%) were treated with antibiotics by 38 family medicine practitioners, 12 pediatricians and 7 general practitioners. 461 (77.2%) patients were <2 years of age. Amoxicillin was administered to 540 (90.5%) patients, with no differences between the various medical specialties. 127/540 (23.5%) patients did not receive the appropriate dosage; 140/413 (33.9%) patients treated with appropriate dosage did not receive the treatment for the appropriate duration of time. 258/357 (72.3%) evaluable patients <2 years of age received an antibiotic considered inappropriate to guidelines (38 not treated with amoxicillin, 94 received inappropriate dosage and 126 not treated for 10 days); 53/100 (53%) evaluable children >2 years of age received an inappropriate antibiotic treatment.
ConclusionsThe majority of primary care physicians treat simple uncomplicated acute otitis media with the recommended antibiotic drug. However, incorrect dosage and shorter than recommended duration of therapy may jeopardize the quality of care in children with simple uncomplicated acute otitis media.
Acute otitis media (AOM) is the most frequent cause of visits to pediatricians in USA.1 More than 50% of the children will have at least one episode of AOM by the age of one year and more than 90% by the age of two years.2,3 The disease is most frequent between 6 and 13 months of age.4 The most frequent bacterial pathogens causing AOM are Streptococcus pneumoniae (40–45% of all culture-positive cases), non-typable Haemophylus influenzae (40–45%), Streptococcus pyogenes (1–5%) and Moraxella catarrhalis (1–5%).4,5
The published guidelines for the treatment of AOM recommend an antibiotic treatment chosen according to the suspected etiologic agent and its presumed susceptibility to antibiotics.6–8 These guidelines were endorsed by Israel in 2006 and 2010,9,10 recommending amoxicillin as first line treatment for AOM, in a dosage of 80–90mg/kg/day and for a duration of 10 days in children <2 years of age and of 5–7 days in children >2 years of age without risk factors.7,8,11 When treatment failures occur, the second choice of antibiotics includes amoxicillin–clavulanate, cefuroxime axetil or intramuscular ceftriaxone.
The objectives of this study were to analyze the adherence to AOM treatment guidelines among primary health care providers in southern Israel, with particular emphasis on the prescribing patterns among various medical specialties and on the adherence to guideline recommendation in respect to the patient age.
Patients and methodsThis was a descriptive prospective study, conducted from January 2003 through May 2004.
SettingThe study was conducted in six primary care pediatric clinics of “Clalit” Health Care Services (CHS) in the city of Beer-Sheva, southern Israel. CHS is the largest Health Maintenance Organization (HMO) in Israel, providing care to >50% of the population in Israel. All clinics recorded patient data on a computerized data system. All physicians participating in the study were employees of CHS and were trained by CHS and also at the department of pediatrics of Soroka University Medical Center, Beer-Sheva.
DefinitionsAOMPresence of acute symptoms and physical signs supporting the diagnosis of AOM.
Simple AOM (s-AOM)<3 AOM episodes during the last six months or <4 episodes during last year and lack of antibiotic treatment for AOM or any other disease during the 72-h period before enrollment.
Complicated AOM≥3 AOM episodes during the last six months or ≥4 episodes during last year and/or administration of an antibiotic treatment for AOM or any other disease during the 72-h period before enrollment.
Adequate dosagemedication dosage ranging from −30% to +30% of the recommended dosage of amoxicillin (80mg/kg/day) according to guidelines.7,8
Under-dosage<70% of the recommended dosage of amoxicillin according to guidelines.
Appropriate duration of therapy10 days of treatment for children <2 years and 5–7 days for patients >2 years.7,10,11
Adherence to therapyTreatment course in which all three criteria (antibiotic selected, adequate dosage and appropriate duration of therapy) were met.
Non-adherence to therapyTreatment in which at least one of the three previous criteria was not met.
Study populationInclusion criteriaAll healthy infants and children living in the city of Beer Sheva aged three months to three years who: (1) were diagnosed with s-AOM by their primary care physicians in the clinics participating in the study and (2) were treated with antibiotics by their primary care physician.
Exclusion criteriaComplicated AOM or any other ear disease.
VariablesIndependent – demographic data such as age, gender, weigh, physician specialty, antibiotics prescribed. Dependent – adherence and non-adherence to the recommended guidelines.
Data collectionData were collected by the principal investigator (NS) and research assistants by reviewing the computerized files system of CHS. The principal investigator or research assistants visited each clinic every 7–10 days and collected patient details within up to 10 days from patient's visit with an AOM diagnosis.
The following information was collected for all children diagnosed with s-AOM:
- (a)
Prescribed antibiotic selected, dosage and duration of therapy.
- (b)
Data on dosage were obtained either directly from the medical file or indirectly calculated by using information available on child's weight and number of antibiotic bottles prescribed.
- (c)
Treating physicians’ training/specialty status (pediatrician specialist, pediatric resident, family medicine physician, general practitioner) and patient details (age, sex, weight).
The study was approved by the Ethics Committee of Soroka University Medical Center.
Data analysisWe used the published guidelines as a reference basis to analyze adherence and non-adherence to recommended treatment.6–9 Data were collected on an Excel electronic worksheet and exported to analysis to SPSS software, version 15.0. A description of qualitative (patient: gender; physician: specialty and type of antibiotic treatment prescribed) and quantitative (patient: age, duration of antibiotics treatment prescribed and dosage) variables was performed. t-Test was used to compare continuous variables and chi-square test for qualitative variables. Data were analyzed according to the guidelines recommended for children under or above 2 years of age.
ResultsOverall, 689 patients were diagnosed with s-AOM. Of them, 92 (13.3%) children were not treated with antibiotics; therefore, the study population included 597 (86.7%) children. These patients were treated with antibiotics by 57 physicians: 38 (66.7%) family medicine physicians, 12 (21%) pediatricians, and 7 (12.3%) general practitioners. Overall, 45.2% (270/597) of the children were treated by a pediatrician. Four hundred and sixty-one (77.2%) of the 597 children were <2 years of age. Five hundred and forty (90.4%) were treated with amoxicillin; of them 413 (69.1%) received an adequate dosage of the medication.
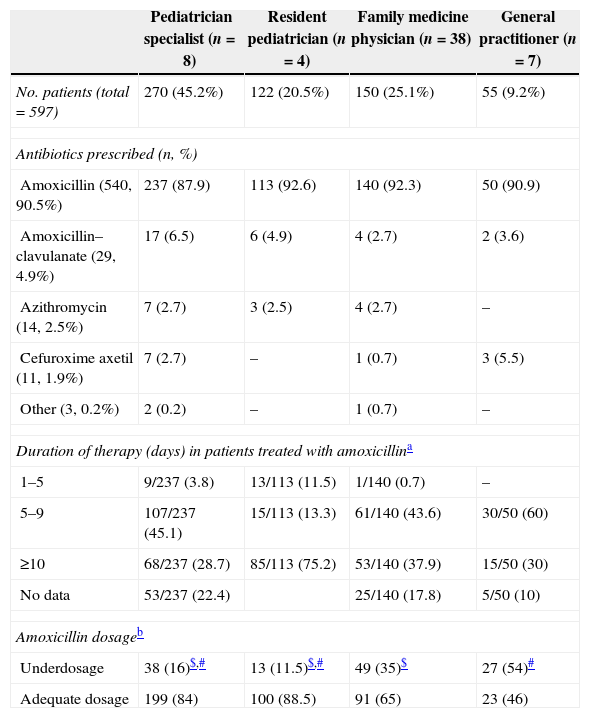
Table 1 describes the antibiotic prescribing characteristics for s-AOM among four groups of prescribing physicians (family medicine, pediatric specialists, pediatric residents and general practitioners). There were no significant differences in the choice of antibiotic therapy among the four groups of physicians. In 31% (168/540) of the cases in which amoxicillin was prescribed the duration of treatment recommended was not mentioned (22.4%, 75.2%, 17.8% and 10% of the patients treated by pediatricians, pediatric residents, family medicine practitioners and general practitioners, respectively). Significantly more patients treated by pediatric residents did not have documentation of the duration of therapy in the medical charts compared to each of the three other specialty categories (p<0.01). More pediatricians (specialists or residents), compared with general practitioners or family medicine practitioners, prescribed the adequate antibiotic dosage as a function of the child's weight and according to the guidelines (85.4% compared with 65% and 46%, respectively, p<0.001).
Antibiotic prescribing patterns for s-AOM, according prescribing physician's specialty.
| Pediatrician specialist (n=8) | Resident pediatrician (n=4) | Family medicine physician (n=38) | General practitioner (n=7) | |
|---|---|---|---|---|
| No. patients (total=597) | 270 (45.2%) | 122 (20.5%) | 150 (25.1%) | 55 (9.2%) |
| Antibiotics prescribed (n, %) | ||||
| Amoxicillin (540, 90.5%) | 237 (87.9) | 113 (92.6) | 140 (92.3) | 50 (90.9) |
| Amoxicillin–clavulanate (29, 4.9%) | 17 (6.5) | 6 (4.9) | 4 (2.7) | 2 (3.6) |
| Azithromycin (14, 2.5%) | 7 (2.7) | 3 (2.5) | 4 (2.7) | – |
| Cefuroxime axetil (11, 1.9%) | 7 (2.7) | – | 1 (0.7) | 3 (5.5) |
| Other (3, 0.2%) | 2 (0.2) | – | 1 (0.7) | – |
| Duration of therapy (days) in patients treated with amoxicillina | ||||
| 1–5 | 9/237 (3.8) | 13/113 (11.5) | 1/140 (0.7) | – |
| 5–9 | 107/237 (45.1) | 15/113 (13.3) | 61/140 (43.6) | 30/50 (60) |
| ≥10 | 68/237 (28.7) | 85/113 (75.2) | 53/140 (37.9) | 15/50 (30) |
| No data | 53/237 (22.4) | 25/140 (17.8) | 5/50 (10) | |
| Amoxicillin dosageb | ||||
| Underdosage | 38 (16)$,# | 13 (11.5)$,# | 49 (35)$ | 27 (54)# |
| Adequate dosage | 199 (84) | 100 (88.5) | 91 (65) | 23 (46) |
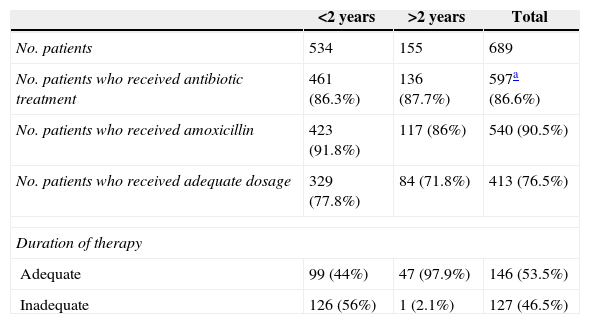
Table 2 describes the characteristics of antibiotic prescription as a function of patient age, drug dosage and duration of therapy. Amoxicillin was the most frequently administered antibiotic in both age groups (in 423 patients <2 years and 117 patients >2 years of age). The adequate dosage of amoxicillin was prescribed in only 329 (77.8%) and 84 (71.8%) for the groups of patients <2 years and >2 years old, respectively.
Amoxicillin prescription for AOM in the community by age groups, dosage and duration of therapy.
| <2 years | >2 years | Total | |
|---|---|---|---|
| No. patients | 534 | 155 | 689 |
| No. patients who received antibiotic treatment | 461 (86.3%) | 136 (87.7%) | 597a (86.6%) |
| No. patients who received amoxicillin | 423 (91.8%) | 117 (86%) | 540 (90.5%) |
| No. patients who received adequate dosage | 329 (77.8%) | 84 (71.8%) | 413 (76.5%) |
| Duration of therapy | |||
| Adequate | 99 (44%) | 47 (97.9%) | 146 (53.5%) |
| Inadequate | 126 (56%) | 1 (2.1%) | 127 (46.5%) |
Duration of therapy was not mentioned in the medical records of 104 patients <2 years of age and 36 patients >2 years of age. While 44% (99/225) of the evaluable patients <2 years of age received an appropriate duration of therapy (10 days), the majority (97.9%, 47/48) of the patients >2 years of age received an appropriate duration of therapy (>5 days for this age group).
In the group of children <2 years old and treated with an adequate dosage of amoxicillin, 2.2% (5/225) of the patients received treatment for 1–4 days only and 53.8% (121/225) received treatment for 5–9 days only. In the group of children >2 years old treated with an adequate dosage of amoxicillin, 2.1% (1/48) received treatment for 1–4 days only and 58.3% (28/48) received treatment for 5–9 days, while 39.6% (19/48) received treatment for 10 days.
DiscussionThe objectives of this study were to analyze the adherence to treatment guidelines of AOM among primary health care providers in primary care health clinics in Southern Israel. We chose to discuss only cases of simple uncomplicated AOM, since the therapeutic decisions regarding cases of recurrent/persistent AOM are more complicated and might be more controversial in respect to diagnosis and treatment.
This study was conducted during 2003–2004, when clinical guidelines regarding treatment of AOM, published by various forums in USA, Europe and also in Israel were recommending treating with antibiotics all children with AOM.7,8 This recommendation was and still is controversial, and in several European countries, including the Netherlands, Belgium and Scandinavian countries, avoiding treating AOM with antibiotics immediately after diagnosis of the disease (in non-toxemic children and without severe disease) was common practice.9,10 Therefore, only 30–50% of the children with AOM in these countries were treated with antibiotics, compared to almost 90% in the USA, Canada, Australia and Israel. During recent years, a reassessment of the guidelines supporting antibiotic administration immediately after diagnosis was made in many countries all over the world, mainly due to the need of limiting antibiotics use and abuse in the treatment of AOM and in order to reduce the high antibiotics resistance rates among the main pathogens causing the disease.11 Therefore, during that period, new guidelines for AOM treatment were established by the American Academy for Pediatrics and American Society of Family Medicine; in Israel, similar recommendations were released.12,13 These guidelines added the recommendation of a 24–48h period of “watchful waiting” without administration of antibiotics in children >6 months age without severe disease, assuming a clinical follow-up could be conducted by the treating physician.
In the present study, we showed that approximately 90% of the physicians in six community clinics in Southern Israel, regardless of their professional background, prescribed amoxicillin as first-line antibiotic treatment for AOM, in accordance with the clinical guidelines published in Israel. This finding reveals that most of these physicians were probably familiar with the clinical guidelines regarding first-line recommended treatment. In contrast, amoxicillin was prescribed for 31–43% of first AOM episodes by medical professionals in the United States.14,15
Only approximately 75% of the physicians participating in the present study prescribed an adequate dosage of amoxicillin. This finding is consistent with published data, reporting that only 74% of the physicians in the United States prescribe an antibiotic dosage consistent with the guidelines recommendations.14
Significantly more pediatricians (specialists or residents), compared to family medicine practitioners and general practitioners, prescribed an adequate dosage of amoxicillin. This finding is also consistent with published literature14 reporting on superior adherence rate to guidelines among pediatricians compared with general practitioners. This may suggest that pediatricians may be more accurate than family medicine practitioners and general practitioners in dosing prescribed drugs according to patient weight. Another possible explanation for this discrepancy may be related to better and more frequent training of pediatricians in southern Israel, contributing to broader knowledge on the appropriate approach to AOM treatment. According to literature reports, physicians’ training is helpful in improving knowledge and antibiotic use patterns.15,16,17 Many physicians participating in the present study did not record in the patient medical charts the recommended duration for antibiotics use. On the other hand, this information could have been conveyed verbally to parents during the visit. Some of the physicians who did not record the recommended duration for antibiotics usage, did prescribe the recommended number of bottles of antibiotics needed; therefore the exact duration of treatment could be ultimately calculated by the authors of the present study. In any case, the fact that 33.9% of the patients treated with amoxicillin (despite receiving an appropriate drug dosage) did not receive treatment for the appropriate duration of therapy, is of major concern.
In regard to appropriateness of treatment to guidelines by age groups, we found that only approximately 25% of the children <2 years of age were treated according to the guidelines in terms of the three main parameters investigated (antibiotic type, dosage and treatment duration). This information is complementary to and broadens recently published data; Garbutt et al.16 reported that an appropriate duration of therapy was prescribed in 98% of the children with AOM receiving amoxicillin (without referral to appropriateness of drug dosages).
It is interesting to point out that the duration of treatment was more adequately prescribed for children >2 years than for children <2 years of age. This may be, most probably, a result of the more liberal recommendations for treatment duration for children >2 years of age and leaving to discretion of the treating physician the option to decide between 5 and 7 days of treatment.6–9 In conclusion, we showed that the majority of the primary care physicians treat s-AOM with the recommended antibiotic drug (amoxicillin). However, inappropriate drug dosage and duration of therapy may jeopardize the quality of care in children with s-AOM.
Conflicts of interestThe authors declare no conflicts of interest.