In physical examination abdominal tenderness, gate disturbance and penile herpetic lesions were detected. Decreased disc height at T11-T12 level was detected in chest X-ray. Abdominal sonography and CT scan revealed hypo dense lesions in Lt left Lobe of liver and multiple hypo dense splenic and pancreatic lesions, ascitis, Lt left sided pleural effusion, thickening of jejuneal mucosa and edema of bowel wall. Vertebral body lesion and paravertebral abscess, bony calvarial involvement and adjacent extra axial brain lesion were observed in imaging were other findings. RNA analysis for HIV was positive. Vertebral lesion biopsy and aspiration of splenic lesion were performed and pathology revealed Pneumocystis jirovecii suggestive of extra pulmonary Pneumocystis carinii infection.
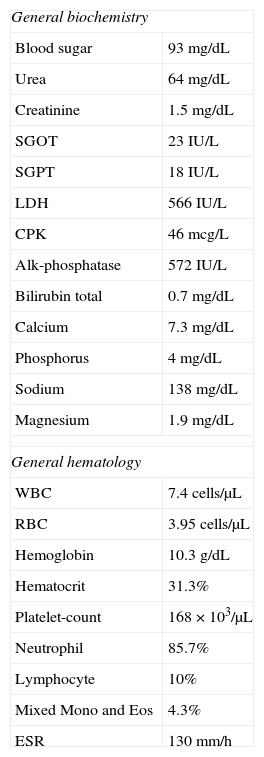
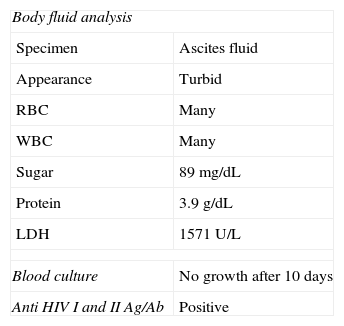
A 46-year old man complaining of dyspnea and abdominal pain since 10 days ago that exacerbated in last 4 days is presented. He mentioned prolonged fever of 39°C, 0.5–1h each night during the last 6 months. The patient was in good general condition. The patient had previously been prescribed anti-TB treatment for suspected tuberculosis in another center based on caseating granuloma found in bone marrow aspiration by pathology and fever had subsided after 48h; however PPD and PCR for TB was not conclusive and HIV test was negative. Besides, there was history of chest wall mass resection reporting well defined capsular structure full of necrotic material destroying underlying bones. On physical examination abdominal tenderness in right upper quadrant, gait disturbance and penile herpetic lesion were detected. He was under treatment with levothyroxin for hypothyroidism and acyclovir for herpetic lesions. CD4 count was 1.8cells/mm3. Laboratory test results are presented in Tables 1 and 2.
General biochemistry and hematology tests.
| General biochemistry | |
| Blood sugar | 93mg/dL |
| Urea | 64mg/dL |
| Creatinine | 1.5mg/dL |
| SGOT | 23IU/L |
| SGPT | 18IU/L |
| LDH | 566IU/L |
| CPK | 46mcg/L |
| Alk-phosphatase | 572IU/L |
| Bilirubin total | 0.7mg/dL |
| Calcium | 7.3mg/dL |
| Phosphorus | 4mg/dL |
| Sodium | 138mg/dL |
| Magnesium | 1.9mg/dL |
| General hematology | |
| WBC | 7.4cells/μL |
| RBC | 3.95cells/μL |
| Hemoglobin | 10.3g/dL |
| Hematocrit | 31.3% |
| Platelet-count | 168×103/μL |
| Neutrophil | 85.7% |
| Lymphocyte | 10% |
| Mixed Mono and Eos | 4.3% |
| ESR | 130mm/h |
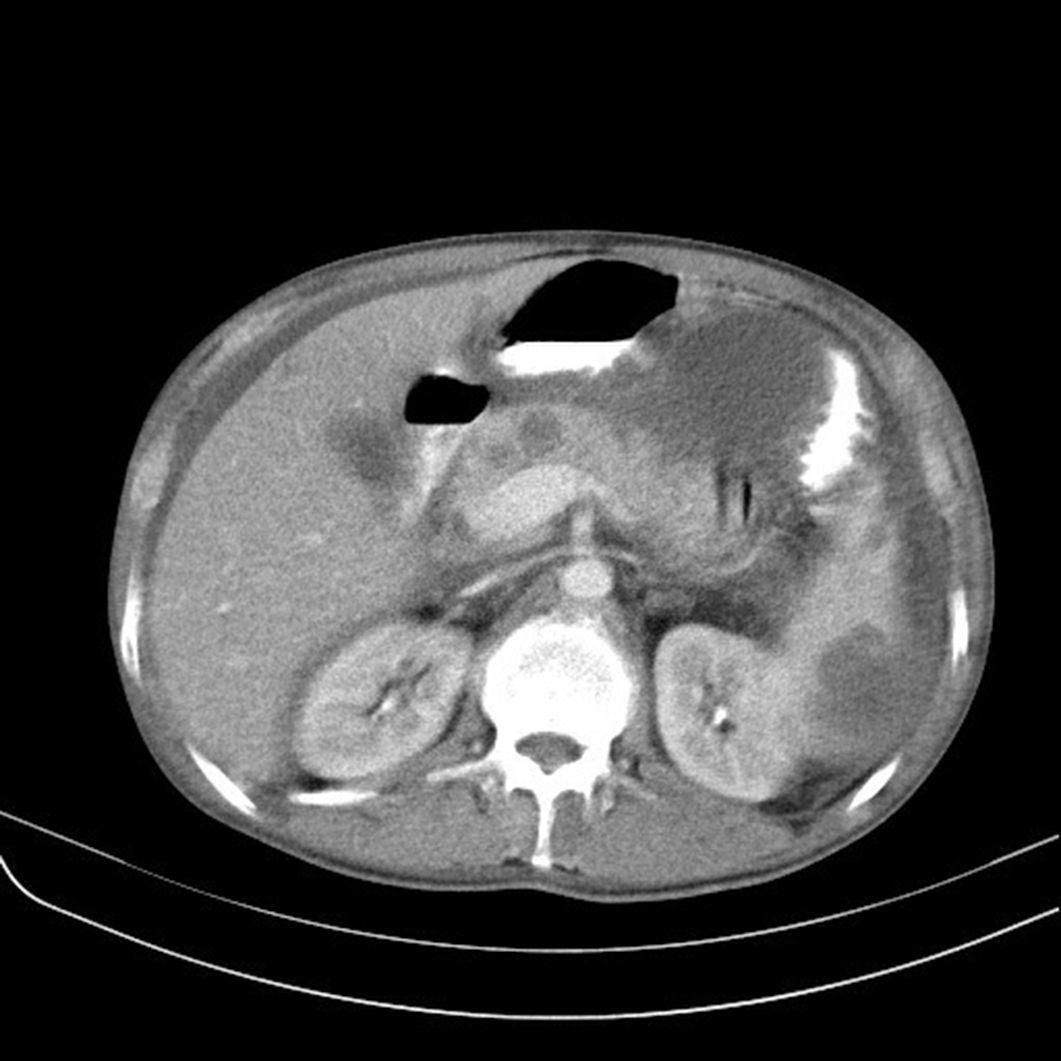
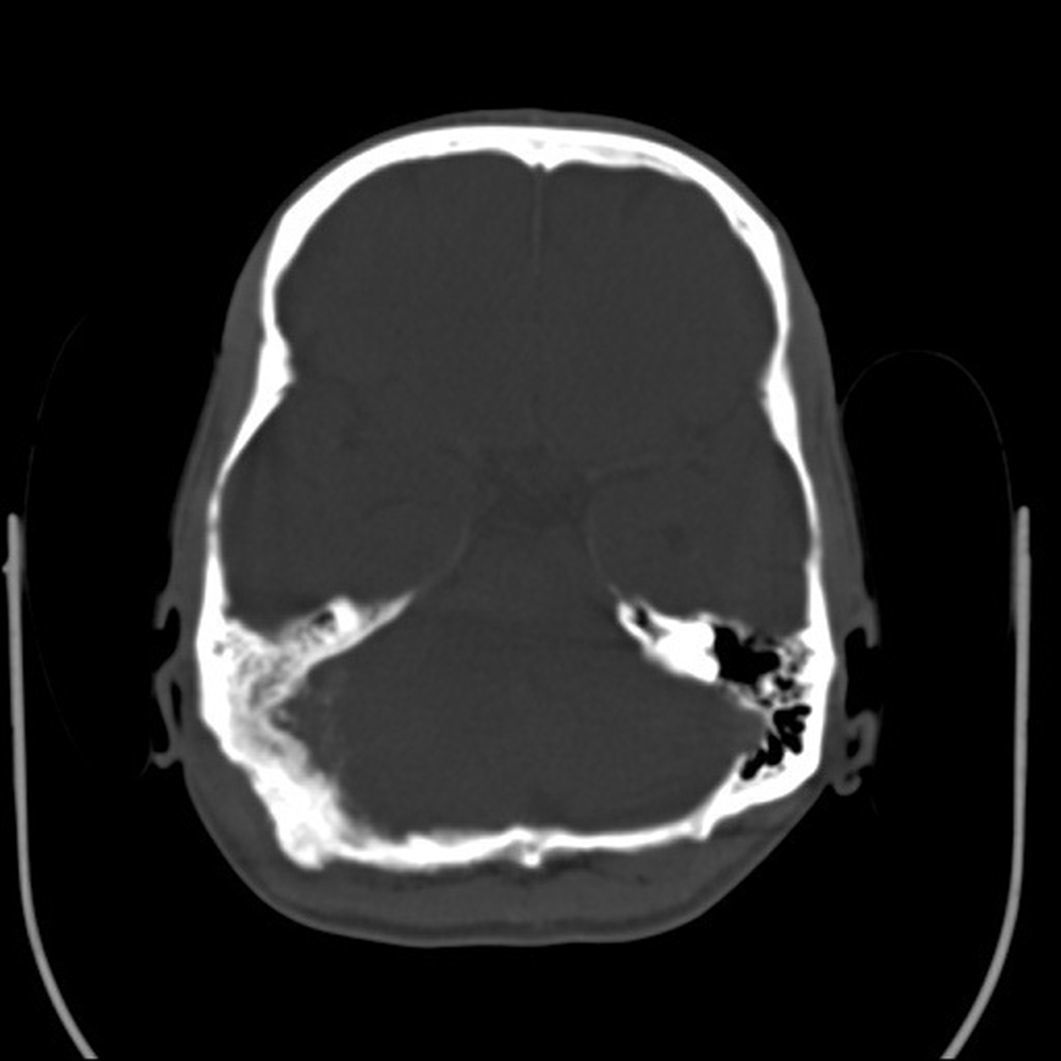
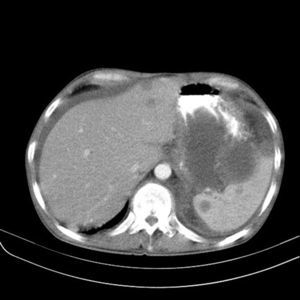
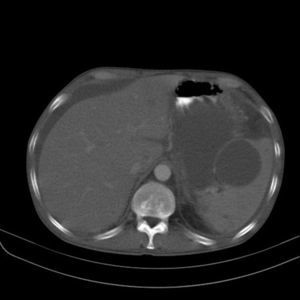
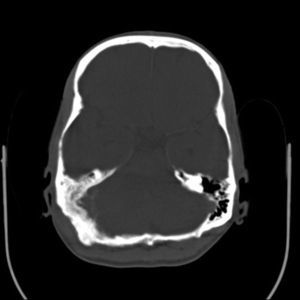
Regarding imaging assessment, abdominal sonography demonstrated ascitis (free fluid in abdomen and pelvic), hypoechoic lesions, calcified lesions and lesions with calcified rim in liver, two similar lesions in pancreas and similar lesions in spleen beside splenomegaly and a 5mm stone and two calcified cyst containing debris in spleen. In chest X-ray (CXR) decreased disk height at T11–T12 level with collapsed T11 vertebral body and paravertebral soft tissue were observed. Abdominal CT showed small sized hypodense lesions in left lobe of liver (Fig. 1), multiple hypodense splenic (Fig. 2) and pancreatic lesions (Fig. 3), left sided pleural effusion, thickening of jejuneal mucosa and edema of bowel wall and ascites (Fig. 4). Vertebral body lesion and paravertebral abscess (Fig. 5), bony calvarial involvement and adjacent extra-axial brain lesion (Fig. 6) are other findings.
Finally, vertebral lesion biopsy and aspiration of splenic lesion were performed and pathology revealed Pneumocystis jiroveci suggestive of extra-pulmonary Pneumocystis infection.
During admission anti TB treatment, HIV treatment and other antibiotics including Ceftriaxone, Metronidazole, Co-trimoxazole, Imipenem and Vancomycin were ordered and Co-trimoxazole, Lamivudine, Zidovudine and Efavirenz were prescribed at discharge.
DiscussionPneumocystis pneumonia (PCP) is the most common opportunistic infection in HIV-infected patients caused by P. jiroveci. This is a life threatening infection in advanced AIDS patients.1 PCP mostly presents as interstitial pneumonia with symptoms like fever, cough, and dyspnea. CXR appearances are mostly seen as bilateral diffuse symmetric finely granular/reticular interstitial/airspace infiltration and most common CT features are patchy work pattern (56%), bilateral asymmetric patchy mosaic appearance.2,3 However, negative CT does not rule out the diagnosis. While PCP is the most prevalent severe pulmonary infection in HIV-infected patients, extra-pulmonary pneumocystosis is almost rare. Extra-pulmonary Pneumocystis infection occurs in HIV-infected patients on pentamidine prophylaxis or in advanced HIV infection without prophylaxis, even without pulmonary involvement. It can affect all organs including central nervous system, bone marrow, lymph node, eye, gastrointestinal tract and thyroid.4 It is mentioned that as a consequence of inadequate concentration of aerosolized pentamidine to suppress systemic infection, it is a contributing factor for extra-pulmonary Pneumocystis infection and as a prophylaxis is insufficient to suppress dissemination.5,6 Low CD4 count, history of other infections, PCP and aerosolized pentamidine prophylaxis are risk factors of extra-pulmonary infection in HIV-infected patients. Extra-pulmonary infection can occur as a complication of PCP.7,8
What makes our case interesting is that he was not recognized as HIV-infected until this infection broke out and only symptoms like fever brought him to the hospital and led to the diagnosis of HIV infection. Even at first laboratory test in other center, the HIV test result was negative. In this previously unrecognized HIV-infected patient, lack of important risk factors like aerosolized pentamidine or previous PCP alongside with absence of any pulmonary imaging findings made diagnosis more difficult.
To best of our knowledge, several extra-pulmonary Pneumocystis cases have been reported in which mostly aerosolized pentamidine was noted as a contributory risk factor. It is also described that recurrent PCP in patients on aerosolized pentamidine is frequent and leads to abnormalities in CXR other than interstitial infiltrate.9–12 In Morlat study, PCP lead to diagnosis of HIV infection in 29 out of 80 patients3 but in this case extra-pulmonary disease without pulmonary findings led to HIV diagnosis. Two extra-pulmonary Pneumocystis infections were reported by Witt et al., 10 one disseminate to liver, spleen and kidney and the other had wide dissemination. Furthermore, Edelstein et al.12 reported that out of 13 cases with history of PCP and on pentamidine prophylaxis, 4 cases showed recurrent PCP and one wide extra-pulmonary dissemination.
The patient presented here had no history of PCP and it was an initial appearance of P. jiroveci infection without any pulmonary imaging findings. Some reports of extra-pulmonary cases without pulmonary involvement are available. Region and colleagues reported an isolated thyroid pneumocystosis without any history of PCP but that case was also known to be HIV infected and on pentamidine prophylaxis.9 Another pneumocystis thyroiditis without pentamidine prophylaxis presented with a neck mass.13 Also, another case of rectal ulcer as initial manifestation of extra-pulmonary disease who was on aerosolized pentamidine and was treated with IV pentamidine. They concluded that low concentration of aerosolized than IV to suppress systemic infection is contributory parameter for extra-pulmonary Pneumocystis.5
An article review which evaluated 37 extra-pulmonary cases of Pneumocystis infection demonstrated that most cases had history of PCP or AIDS related infections. Pathological evaluation suggests that most cases had hematogenous and lymphatic dissemination from the lung.14 Considering cases similar to ours, in 2007 a patient with multiskeletal and gastrointestinal involvement was reported. There was a pulmonary mass of which cytology was unrevealing and the diagnosis of P. jiroveci was made from sternal aspiration cytology. Another HIV-infected case complaining of fever was also reported with extra-pulmonary P. jiroveci infection detected at the spleen without any pulmonary involvement.15 Considering bone and gastric tract involvement in our case and similar cases, like the case reported in 2007 by Panos,16 the diagnosis of pnemocystosis should be kept in mind as a differential diagnosis when these symptoms come together. Lymphadenopathy also is assumed not uncommon in extra-pulmonary Pneumocystis. In 2007, a 9-year old HIV-infected boy presented with generalized lymphadenopathy and fine needle aspiration cytology showed extra-pulmonary Pneumocystis infection.7,15
P. jiroveci infection, the most common severe infection and particularly lethal in HIV-infected patients, should be carefully observed. Although diagnosing and treating PCP is not difficult, in case of dissemination survival is particularly poor, possibly because clinicians are unaware of complications of delayed treatment.6 Hematogenous and lymphatic dissemination from lung, reactivation of latent infection in extra-pulmonary sites or primary infection of those sites are identified as dissemination pathways based on pathology as reported by Cohen and Stoeckle14 in a study of 37 cases.
The key to diagnosis of extra-pulmonary pneumocystosis is the support of clinical microbiology and pathology. A histological examination that reveals an eosinophilic, foamy substance surrounding cyst walls and/or trophozoites in affected tissues is generally regarded as the primary diagnostic method for extra-pulmonary pneumocystosis.15 Diagnostic imaging usually can diagnose P. jiroveci in lung and CT should be quite useful in diagnosing extra-pulmonary infections as the incidence of extra-pulmonary Pneumocystis is increasing.17
Some presentations of extra-pulmonary pnemocystosis are focal low attenuation splenic lesions that becomes progressively calcified; punctuate calcification in the liver, renal cortex and adrenal glands; lymph node calcification, and pleural and peritoneal effusion with subsequent calcification in the surface18 Enlarged heterogeneous spleen with innumerable, low attenuation, hypodense lesions; hepatomegaly; gallbladder wall thickening are some findings reported in extrapulmonary pnemocystosis, as well.15 CXR of our case demonstrated decreased disk height at T11–T12 level with collapsed T11 vertebral body and paravertebral soft tissue. Abdominal CT findings of our case consisted of small sized hypodense lesions in left lobe of liver and multiple hypodense splenic and pancreas lesions, ascitis and left sided pleural effusion, thickening of jejuneal mucosa and edema of bowel wall and ascitis. Vertebral body lesion and paravertebral abscess, bony calvarial involvement and adjacent extra-axial brain lesion are other findings.
However it is hypothesized that PCP and extra-pulmonary Pneumocystis infection are caused by genetic variants of P. jiroveci that may potentially differ in their susceptibility to therapeutic regimens; nonetheless, the standard of treatment for extra-pulmonary infection remains similar to that of PCP.15
To sum up, in face of increasing HIV epidemic and consequently P. jiroveci infection in our country and role of early diagnosis in survival of disseminated cases, it is very important for radiologists to be aware of suspicious imaging findings of extra-pulmonary pneumocystosis when it comes to differential diagnosis especially in HIV-infected cases. However, as it happened in our case, it can be the initial manifestation leading to HIV diagnosis, surprisingly.
Conflicts of interestThe authors declare no conflicts of interest.