Tuberculosis verrucosa cutis is a rare medical condition that is caused by the inoculation of Mycobacterium tuberculosis into the skin of a previously sensitized individual. This clinical form of tuberculosis corresponds to 1–2% of all cases of tuberculosis and due to the paucibacillary characteristic of the lesions, patients can be misdiagnosed, accounting for the chronification of the skin infection. Herein, we report the case of a 26-year-old male farmer, presenting plaques with verrucosa and hyperkeratosis features in the left thigh and buttocks during 15 years. M. tuberculosis was identified by PCR and the patient was treated with standard anti-tuberculosis drugs, with subsequent improvement of the skin lesions.
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis, that preferentially affects the lungs. Extrapulmonary tuberculosis manifestation is considered uncommon and accounts for approximately 10% of cases, affecting the central nervous system, kidney, urinary and gastrointestinal tracts; cutaneous involvement occurs in 1–2% of all extrapulmonary tuberculosis manifestations, and can be caused by M. bovis.1,2 Although rare, cutaneous tuberculosis presents clinical variants, classified according to the morphological patterns of the lesions, route of acquisition, and host immune status.3
Tuberculosis verrucosa cutis occurs in previously sensitized patients, and it is a result of a direct inoculation of M. tuberculosis bacillus.2,4 This clinical form of tuberculosis is frequently observed in children, and skin lesions frequently develop in the extremities; among adults it is associated with occupational exposure, and the fingers, hands, ankles or buttocks are affected sites. Primary inoculation tuberculosis occurs after inoculation of M. tuberculosis bacillus into the skin of individuals not previously sensitized, thus without immunity to the bacillus. At the site of entry, inflammatory papules develop and evolve into a firm, shallow, nontender, nonhealing, undermined ulcer with a granulomatous base. This clinical form may resolve or progress to the disseminated form, with the bacillus spreading to other organs.4
Scrofuloderma is caused by M. tuberculosis or M. bovis and it results from the direct extension of the infection from a deep structure (e.g., lymph node or bone), into the overlying skin, and it can be characterized by a subcutaneous lesion that is painless and the nodules can evolve to ulcers and fistulous with drainage of serous, purulent or caseous content. The neck, axillae, or groin are common areas of involvement.5 Tuberculosis cutis orificialis occurs in immunocompromised adults with advanced pulmonary, gastrointestinal, or genitourinary tuberculosis, and the nasal, oral, or anogenital skin or mucosa areas can be affected after autoinoculation of the bacillus in such areas.5
Lupus vulgaris is the most common form of cutaneous tuberculosis, and it can be acquired by inoculation of the bacillus into the skin or endogenously by hematogenous or lymphatic spread in individuals with moderate or high degree of immunity. This clinical form manifests mostly in women, as latent nodules and annular plaques, or it may present with hypertrophic or vegetative lesions; lower extremities or buttocks are frequently affected areas.6 Hematogenous metastatic tuberculous abscess occurs in immunocompromised patients that present single or multiple subcutaneous nodules, that can develop into ulcers or draining sinuses without regional adenopathy. This variant of cutaneous tuberculosis can appear as cellulitis or as purpuric papules that may become umbilicated and crusted.7
Herein, we describe a patient with tuberculosis verrucosa cutis with an evolution of 15 years. Importantly, this type of lesion is unusual and frequently is associated with the activities of anatomists, physicians and bare-footed children living in tropical regions.6
Case reportA 26-year-old male farmer, residing in Belém, Pará State, Brazil, presented to the outpatient service of Dermatology Division, Clinical Hospital, São Paulo University, Brazil, showing a verrucous plaque in the both buttocks, and in the left thigh (Fig. 1A and B). Fistulous areas with drainage of a small amount of purulent content were noted in the left buttock. Inguinal lymphadenomegaly was not observed. The patient reported that the lesions started 15 years ago and increased in size and thickness slowly over time with local pruritus. In other medical services, he was treated with topical and oral drugs such as corticosteroids, antimycotics, antiallergics with no improvement. Additionally, none in his family presented similar lesions.
A 26-year-old male farmer presented a verrucous plaque in the left side of the buttock (A), that spread to the right one (B). A marked improvement of the skin lesions caused by M. tuberculosis was observed after treatment, performed with rifampicin, isoniazid, pyrazinamide and ethambutol during six months.
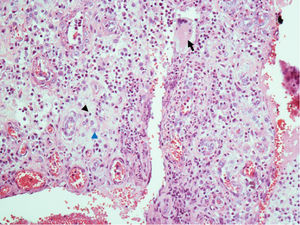
Blood-biochemical parameters were within normal ranges, and the patient tested negative for HIV, B and C hepatitis, and syphilis. Thoracic and abdominal radiography and ultrasonographic examination were normal. Mantoux test, performed with 5UI of tuberculin protein, was positive after 48 h of inoculation and showed a diameter higher than 20 mm. Biopsies were collected in three different regions from the left buttock, and the histological sections were stained with hematoxylin-eosin (HE) and Ziehl-Neelsen technique to evidence acid-alcohol resistant bacilli. Fragments of the skin were cultured in Lowenstein-Jensen medium, and polymerase chain reaction (PCR) was used to identify the etiologic agent.8–10
The histological section of the skin stained with HE showed intense hyperkeratosis with accentuated papillomatosis. The dermal inflammatory infiltrate was characterized by the presence of lymphocytes, histiocytes, Langerhans cells, neutrophils and giant cells; granulomas were observed in the skin histological sections, but no caseous necrosis was observed (Fig. 2). No bacilli were grown in the culture of the skin fragments nor were seen in sections stained with Ziehl-Neelsen technique. In spite of that, M. tuberculosis bacilli were identified by PCR. The patient was treated with rifampicin, isoniazid, pyrazinamide and ethambutol for six months, according to the recommendations of the Ministry of Health of Brazil.10 This patient has been follwed monthly, and clinical improvement during treatment has been observed (Fig. 1C).
ConclusionTuberculosis is associated with precarious social and economic conditions, and has been considered a reemerging disease caused by a set of reasons, such as poverty, malnutrition, high HIV incidence, use of immunosuppressant drugs, and existence of resistant bacilli.11 Furthermore, there are different clinical forms that are difficult to be diagnosed,12 and consequently the mycobacteria coexists with the patient during a long period of time, contacting different classes of drugs that may favor the emergence of resistant strains.
Cutaneous manifestations of tuberculosis have been considered as a rare event, making the diagnosis a challenge. In patients with tuberculosis verrucosa cutis, where the individual was already sensitized by the bacillus, there is no ganglionar involvement, but the tuberculin intradermal test is frequently positive, as observed in the above-mentioned patient. Despite immunological positivity, the number of bacilli in culture is low, and histological sections stained with Ziehl-Neelsen technique are negative.13 These findings are relatively frequent due to the paucibacillary nature of the lesions at the dermal site of infection. However, the use of the PCR technique may improve diagnosis,10 as observed herein. Although considered expansive, this technique may speed up the treatment of patients, and importantly, avoid the misdiagnosis of cutaneous tuberculosis.
Therefore, in medical services without the possibility of performing PCR, the diagnosis may consider the features of cutaneous lesions, and at the same time it becomes important to carry out a differential diagnosis with other medical conditions that affect the skin, such as leishmaniasis and chromoblastomycosis,14,15 avoiding misdiagnosis and consequently disease progression, as observed in the patient studied by us.
The present case report highlights the importance of an early diagnosis of cutaneous tuberculosis, avoiding the occurrence of chronic and exuberant cases as described above, whose diagnosis was neglected during 15 years. Although only a few cases with lesions for more than 20 years have been reported in the medical literature, no functional disability has been detected. However, it is still important to highlight that this disease progresses slowly, and persists if not properly treated,16,17 as observed in this patient that coexisted with the etiologic agent for more than 50% of his life span.
The authors would like to thank HCFMUSP-LIM50.