Brucellosis is one of the most common zoonotic infection worldwide and endemic in Turkey. It constitutes an important public health problem, especially in rural areas. Brucellosis primarily occurs in animals and it is transmitted to humans by direct contact with infected animals or ingestion of unpasteurized milk and milk products.1
Brucellosis is a multisystem disease and the clinical features of brucellosis vary greatly. Neurobrucellosis is a rare complication in childhood which can be detected in 2–7 percent of cases. The most common clinical forms of neurobrucellosis are meningitis, encephalitis, and myelitis while brucellar brain abscess is extremely rare.2 Here, an eight-year-old girl with afebrile seizures due to brucellar brain abscess is presented to emphasize different clinical manifestations of brucellosis in endemic areas.
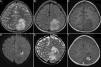
An eight-year-old girl was admitted to our hospital with complaints of vomiting and afebrile seizures. Her history revealed malaise, loss of appetite, and recurrent afebrile generalized tonic seizures lasting for 8–10min in the past month. Her medical history was unremarkable with no history of trauma. On admission, she had no fever, nor any neurological deficits and the systemic examination was unremarkable except for a systolic murmur. Laboratory tests included complete blood count and blood chemistry within normal limits except for an elevated C-reactive protein (CRP) of 74mg/L. Electrocardiography (ECG) and echocardiography were normal. The awake and asleep EEG revealed slowing of background rhythm over the left parieto-occipital area with no epileptiform discharges. She had two episodes of afebrile generalized tonic seizures at the time of hospitalization and phenytoin was started. Cranial magnetic resonance imaging (MRI) showed a multiloculated lesion 50mm×40mm in size, hypointense on T1 and hyperintense on both T2 and fluid-attenuated inversion recovery (FLAIR) images at the left parieto-occipital region with peripheral edema. Contrast enhancement was also suggestive of an abscess formation (Fig. 1). Lumbar puncture was not performed because of the large mass compatible with brain abscess and the surrounding extensive edema. Ceftriaxone, metronidazole, and mannitol were added. The case underwent burr hole drainage and 40mL of purulent material was drained. One month after the first procedure, parieto-occipital craniotomy was performed to evacuate the abscess that had recurred. No microorganisms were isolated from the abscess cultures. Blood cultures and serological test for hydatid cysts were negative. Brucella agglutination test was positive at 1:1280 titers in blood. When the patient's history was questioned in detail, it was learned that her family was living in the countryside, her father was a farmer and brucellosis has been diagnosed in one of her sisters. Intravenous ceftriaxone was given for 10 days followed by oral rifampicin and trimethoprim-sulfamethoxazole. The blood brucella agglutination titer was 1:320 at the second month and long-term antibiotic treatment was planned with rifampicin and trimethoprim-sulfamethoxazole.
Axial T2-weighted (A) and FLAIR images (B) revealing hyperintense cortical-subcortical 50mm×40mm lesion with surrounding edema. Axial T1-weighted (C), diffusion-weighted (DWI) (D), apparent-diffusion coefficient (E) and T1-weighted post-contrast images with peripheral ring-like enhancement (F) confirming abscess formation.
Human brucellosis is a multisystemic infectious disease and is an important cause of morbidity in endemic areas. Severe complications can develop in cases of delayed diagnosis and inadequate treatment. Neurobrucellosis is a severe but rarely seen complication of human brucellosis. Meningitis is the most common clinical form of the disease. Brain abscess due to neurobrucellosis is extremely rare in childhood.3 A few case reports of multiple abscesses in brain parenchyma due to neurobrucellosis in childhood have been reported in the literature.3
Patients with neurobrucellosis can present with fever, neck stiffness, confusion, vomiting, headache, cranial nerve paralysis, aphasia, psychiatric symptoms (agitation, personality disorder, depression, psychosis), ataxia, and seizures.4 Some patients present with a neurological disorder without systemic signs or symptoms. Because of the lack of pathognomonic signs and symptoms, clinical suspicion plays a key role in endemic areas. Clinical diagnosis should be confirmed by bacteriology or serology and cerebrospinal fluid analysis. A prolonged (at least 4–6 months) combined antibiotic treatment including two or three drugs that cross the blood–brain barrier is recommended for treating neurobrucellosis. Doxycycline, rifampin, and either ceftriaxone or trimethoprim-sulfamethoxazole are the most commonly used treatment regimens.4,5 Ceftriaxone-based regimens were found to be more successful and requiring shorter duration of therapy.5
In conclusion, although rare, neurobrucellosis and brucellar brain abscess should be kept in mind in the differential diagnosis of various neurological symptoms including afebrile seizures especially in endemic areas.
Conflicts of interestThe authors declare no conflicts of interest.