Two-Drug Regimens (2DR) have proven effective in clinical trials but real-world data, especially in resource-limited settings, is limited.
ObjectivesTo evaluate viral suppression of lamivudine-based 2DR, with dolutegravir or ritonavir-boosted protease inhibitor (lopinavir/r, atazanavir/r or darunavir/r), among all cases regardless of selection criteria.
Patients and methodsA retrospective study, conducted in an HIV clinic in the metropolitan area of São Paulo, Brazil. Per-protocol failure was defined as viremia above 200 copies/mL at outcome. Intention-To-Treat-Exposed (ITT-E) failure was considered for those who initiated 2DR but subsequently had either (i) Delay over 30 days in Antiretroviral Treatment (ART) dispensation, (ii) ART changed or (iii) Viremia > 200 copies/mL in the last observation using 2DR.
ResultsOut of 278 patients initiating 2DR, 99.6% had viremia below 200 copies/mL at last observation, 97.8% below 50 copies/mL. Lamivudine resistance, either documented (M184V) or presumed (viremia > 200 copies/mL over a month using 3TC) was present in 11% of cases that showed lower suppression rates (97%), but with no significant hazard ratio to fail per ITT-E (1.24, p = 0.78). Decreased kidney function, present in 18 cases, showed of 4.69 hazard ratio (p = 0.02) per ITT-E for failure (3/18). As per protocol analysis, three failures occurred, none with renal dysfunction.
ConclusionsThe 2DR is feasible, with robust suppression rates, even when 3TC resistance or renal dysfunction is present, and close monitoring of these cases may guarantee long-term suppression.
Antiretroviral therapy has changed AIDS since High-Active Antiretroviral Therapy (HAART) was introduced in the late 90′. From complex posology and sub-optimal potency, antiretroviral armamentarium has evolved markedly in the last 20+years, allowing People Living With HIV (PLWH) to have normal lives. Triple therapy has been the pillar of an adequate combination, using thereof available medications to provide a safe viral control.1 Triple therapy is supported by many studies, usually combining two Nucleos(t)ide analog Reverse Transcriptase Inhibitor (NRTI) with a third drug from a different class; Non-Nucleoside Reverse Transcriptase Inhibitor (NNRTI), a Protease Inhibitor (PI), and more recently integrase inhibitor (INI). Single or dual therapy in the same class, even of newer, second-generation drugs, showed the inability to offer adequate viral suppression.2,3
Reducing pill burden and avoiding drug exposure (toxicity) has led to the evaluation of a new dual therapy modality, not the original two NRTI regimens from the pre-HAART era, but combining two classes, as lamivudine (3TC) with protease inhibitor,4-6 or second generation INI with NRTI7,8 or NNRTI.9,10 Used either as initial therapy4 or as a simplification for virally suppressed individuals,5,11 two-Drug antiretroviral Regimens (2DR) are now recommended in many situations.12 Real-world data on the impact of policies, especially from resource-limited settings, is still limited. This study presents the monitoring of 2DR use in public service in Brazil to evaluate viral suppression and potential factors associated with viral failure in a real-world situation, that included cases where 2DR was initiated without all formal criteria of the recommended protocols.13,14
Patients and methodsWe conducted a retrospective study at CME-I (Santo André Infectious Diseases Outpatient Clinic), a metropolitan area of São Paulo, Brazil. This evaluation includes all patients living with HIV (PLWH) in 2DR registered in the official electronic medication dispensing system (SICLOM, Sistema Brasileiro de Controle Logístico de Medicamentos) from 2015 to 2021. Two Drug Antiretroviral regimens (2DR) were defined, for this study, as the association of two classes, 3TC 300 mg per day as an NRTI with; either (i) The integrase inhibitor dolutegravir 50 mg per day or (ii) A ritonavir-boosted protease inhibitor (PIr, lopinavir 400 mg/ritonavir 100 mg twice a day, atazanavir 300 mg/ritonavir 100 mg once a day or darunavir 600 mg/ritonavir 100 mg twice a day). The option to switch to 2DR was made by the attending physician, sometimes without all formal criteria recommended by official protocols, such as antiretroviral treatment for more than 6-months, genotyping without lamivudine and integrase resistance mutation,13,14 or renal dysfunction.
All available medical record with enrollment information was evaluated. For patients without CD4+ T-cells count and HIV-1 viral load from the day of diagnosis results from the first 6-months pre-ART were considered.
Genotypic lamivudine resistance (e.g., M184V/I) previous to 2DR initiation was documented in some cases, or inferred from a history of virological failure, defined as at least one viral load determination above 200 copies/mL in the use of lamivudine (3TC resistance group) for over one month. Cases without a documented virological failure using 3TC or a genotypic resistant test were assumed to be as without 3TC resistance (3TC susceptible group). Cases without documented viral load information during the entire follow-up period were described as missing (unknown group).
Information on co-morbidities that may have contributed to the indication of 2DR was sought in the medical records, including data on renal function, as well as osteoporosis, osteopenia, dyslipidemia, systemic arterial hypertension, depression, and diabetes mellitus. The glomerular filtration rate was estimated using CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration), both before the start of 2DR and at the last observation. Decreased kidney function was defined as Glomerular Filtration Rate (GFR) < 60 mL/min/1.73 m2 and kidney failure if GFR < 15 mL/min/1.73 m2 or dialysis treatment.15
End pointsThe primary objective of the study was to document the overall viral suppression rates of 2DR regimens. A secondary objective was to evaluate the impact of previous 3TC failure and renal dysfunction, estimated by the CKD-EPI. Per-protocol failure was defined as a viral load above 200 copies/mL at the last observation of patients using the 2DR regimen regularly, that started 2DR with undetected viral load. Intention-To-Treat-Exposed (ITT-E) failure was considered for any participants who started 2DR but had either: (i) Delay (> 30 days) in ART dispensation (for any reason, including death, loss to follow-up), (ii) ART change to another regimen (no defined as 2DR) or (iii) Viral load above 200 copies/mL in the last observation. In addition, a snapshot at 48-weeks was performed using viral load above or below 50 copies/mL, considering viral load testing collected from 48 up to 60 weeks on 2DR.
ART delay was calculated by checking the SICLOM on March 3, 2022, adding the date of the last ART withdrawal, and the number of days of medication dispensed, resulting in a deadline for a new withdrawal, with a tolerance of 30 days.
Definition of periodsTime of follow-up in 2DR was considered from the start of 2DR to the last viral load available on 2DR, last checked on April 2022.
Time total on ART was calculated from the beginning of the first ART to the date of the last ARV withdrawal, plus the number of days of ART dispensed.
Time in ART until starting 2DR was calculated from the start of the first ART to the 2DR start date.
Time in viral suppression, time before the start of 2DR, considered from the first recorded viral load < 50 copies/mL to date of 2DR start, whenever a continuous period without any test result above 200 copies/mL.
Time in use of 3TC ‒ 150 mg/day was considered from the start of lamivudine 150 mg per day to the chance of dose or last observation on April 7, 2022.
Statistical analysisStatistical analyzes were performed with Stata version 14.2 (Stata Corp LLC, College Station, Texas, USA) and IBM SPSS Statistics for Windows, Version 24.0. (Armonk, NY: IBM Corp.). The results of continuous variables were expressed in medians, with the 25th and 75th percentiles (IQR) or as a 95% Confidence Interval (95% CI). A significant level of p < 0.05, two-tailed, was applied to all analyses. Variables were compared (3TC resistance vs. 3TC Susceptible), using Mann-Whitney or Kruskal-Wallis test for continuous variables and Chi-Squared (χ2) or Fisher's exact test for categorical variables, as appropriate, and Cox proportional-hazards model to assess failure per Intent-To Treat-Exposed (ITT-E). Survival time was defined as the time (days) from the date of onset of 2DR to the date of the last viral load test available using 2DR, censored on April 7, 2022. To evaluate associated factors, we included demographic and clinical variables (unadjusted), such as sex (male), gender (transwomen), Men who have Sex with Men (MSM), race (white), degree of education (college degree), age at start 2DR (years), viral load > 100,000 copies/mL and late diagnostic (CD4+ T-cells count < 200 cells/mm3) at the diagnosis. Variables with a p-value < 0.20 were included in the adjusted Cox analysis.
EthicsThe study was approved by the institutional ethical committee (CAAE: 21164819.7.0000.0082) and participants provided informed consent.
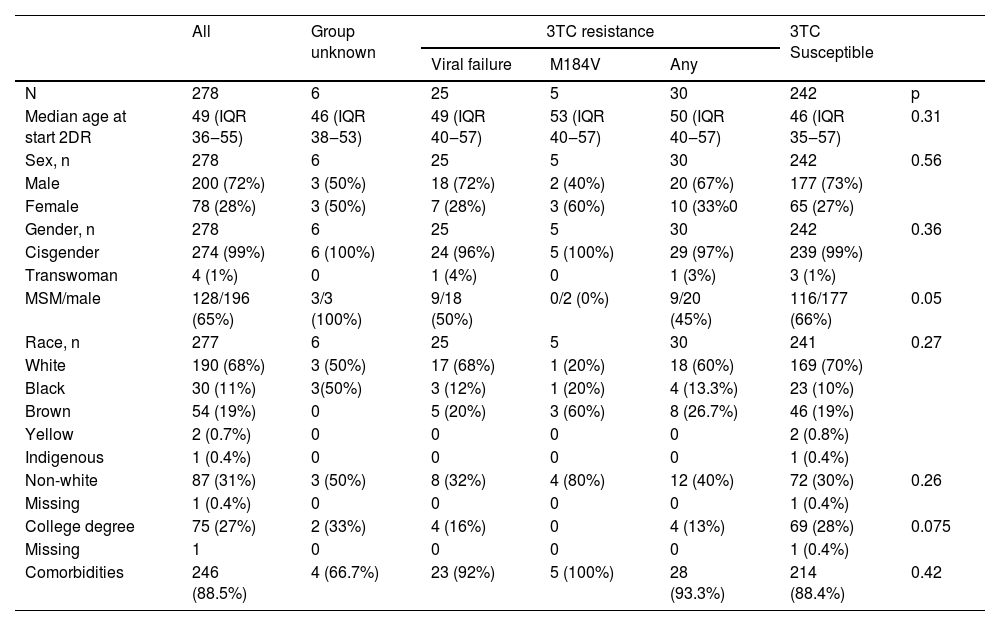
ResultsFrom August 2015 to September 2021, 282 patients started 2DR. Four cases were excluded from the analysis because, despite the regular use of 2DR at SICLOM, no medical records were available. Of the 278 cases analyzed, most were cisgender white, middle-aged males and Men who have Sex with Men (MSM). Table 1 summarizes the socio-demographic and Table 2 laboratory characteristics of these cases, stratified according to documented or presumed 3TC resistance. Only 65 cases had HIV drug resistance genotyping available before the initiation of 2DR. Lamivudine resistance was documented in 5 cases, all with the M184V resistance mutation. Resistance to 3TC was inferred for 25 additional cases.
Socio-demographic data at admission stratified according to 3TC susceptibility.
3TC, Lamivudine; 2DR, Two-Drug Regimens; MSM, Men who have Sex with Men; Group 3TC susceptible, cases without documented viremia > 200 copies/mL using 3TC, prior to initiation of 2DR; Group 3TC resistance, M184V, documented 3TC resistance by genotyping (Stanford db) or Viral failure, resistance presumed by virological failure (viremia > 200 copies/mL using 3TC), prior to initiation of 2DR. Group unknown, cases with periods with no documented viral load. Values are presented as the number of cases and proportion. Continuous variables are expressed as the median and interquartile range (IQR 25%‒75%). Variables were compared using the Mann-Whitney test for continuous variables, and Kruskal-Wallis to race, and Chi-Squared (χ2) or Fisher's exact tests for categorical variables, as appropriate (any 3TC resistance vs. 3TC susceptible).
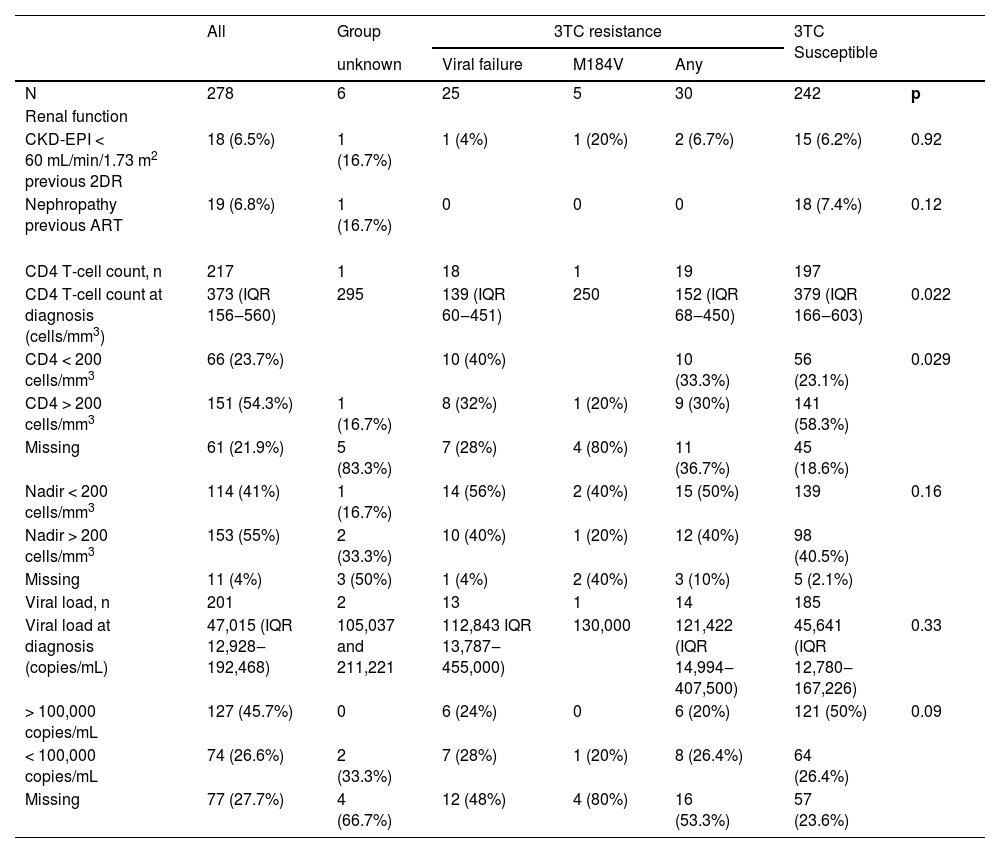
Laboratory data at admission stratified according to 3TC resistance.
3TC, Lamivudine; 2DR, two-Drug Regimens; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; ART, Antiretroviral Therapy; Group 3TC susceptible, cases without documented viremia > 200 copies/mL using 3TC, prior to initiation of 2DR; Group 3TC resistance, M184V/I, documented 3TC resistance by genotyping (Stanford db) or Viral failure, resistance presumed by virological failure (viremia > 200 copies/mL using 3TC), prior to initiation of 2DR. Group unknown, cases with periods with no documented viral load. Values are presented as number of cases and proportion. Continuous variables are expressed as the median and interquartile range (IQR 25%‒75%). Variables were compared using Mann-Whitney test for continuous variables and Chi-Squared (χ2) or Fisher's exact tests for categorical variables, as appropriate (any 3TC resistance vs. 3TC susceptible).
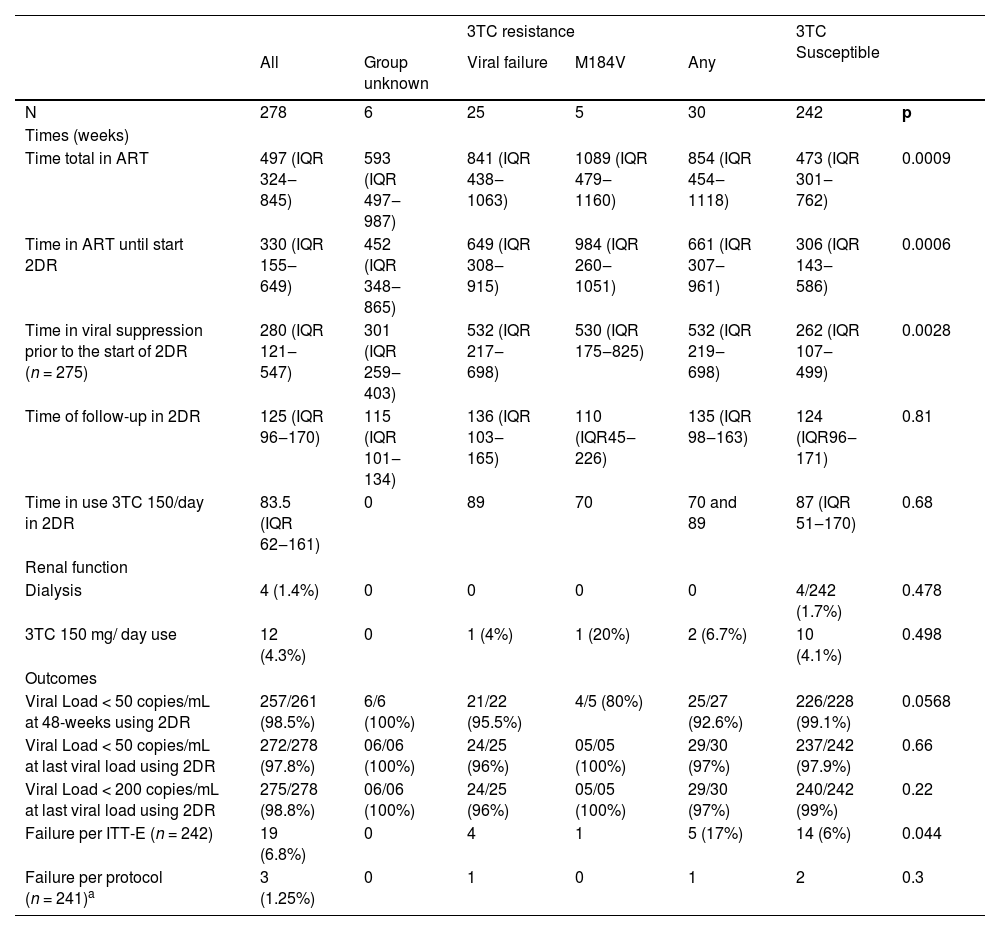
ART was used for a median of 6.9 years (330 weeks, IQR 155‒649) before 2DR initiation and suppressed for 5.8 years (280 weeks, IQR 121‒547), with only one initiating 2DR ARV naïve (Table 3). Most (206, 74%) started 2DR with 3TC+dolutegravir, 41 (15%) with 3TC+atazanavir/ritonavir, 22 (8%) with 3TC+darunavir/ritonavir and 9 (3%) with 3TC+lopinavir/ritonavir.
Outcomes of two-drug regimens, stratified according to documented or presumed 3TC resistance.
3TC, Lmivudine; 2DR, two-Drug Regimens; ART, Antiretroviral Therapy; Group 3TC susceptible, cases without documented viremia > 200 copies/mL using 3TC, prior to initiation of 2DR; Group 3TC resistance, M184V, documented 3TC resistance by genotyping (Stanford db) or Viral failure, resistance presumed by virological failure (viremia > 200 copies/mL using 3TC), prior to initiation of 2DR. Group unknown, cases with periods with no documented viral load; Time total in ART, calculated from the beginning of the first ART regimen to the date of the last ART withdrawal, plus the number of days of ART dispensed, Time in ART until start 2DR, calculated from the start of the first ARV regimen to the 2DR start date; Time in viral suppression prior to the start of 2DR, time of continuous period from the first record of viral load < 50 copies/mL, without any record > 200 copies/mL. Time of follow-up in 2DR, from the beginning of the 2DR until the last viral load available in 2DR, verified in April 2022; Time of use 3TC 150/day in 2DR, was considered to be between the start of lamivudine 150 mg/day to the end or April 7, 2022; Failure per Intent To Treat (ITT-E), considered in all participants who started 2DR considering failure delays in ART withdrawal, death, loss of follow up, ART change (not defined as 2DR), or viral load > 200 copies/mL in the last collection on 2DR; Failure per-protocol, defined if at the last collection, using regular 2DR, had a viral load > 200 copies/mL was verified in a patient who switched to 2DR, with no viremia detected at the time of this switch.
aOne case started 2DR as a first regimen, without viral suppression and was not included. Values are presented as the number of cases and proportion. Continuous variables are expressed as the median and interquartile range (IQR 25%‒75%). Variables were compared using the Mann-Whitney test for continuous variables and Chi-Squared (χ2) or Fisher's exact tests for categorical variables, as appropriate (any 3TC resistance vs. 3TC susceptible).
The most prevalent reported co-morbidity was osteoporosis/osteopenia 174 (62.6%), followed by dyslipidemia 94 (33.8%), hypertension 55 (19.8%), depression 38 (13.7%), diabetes mellitus 26 (9.4%) and nephropathy 19 (6.8%).
CKD-EPI less than 60 mL/min/1.73 m2 was verified at the start of 2DR in 18 patients. Four of these 18 underwent hemodialysis, two of which started 3TC+dolutegravir during hemodialysis. In 2/4 cases that reversed severe renal failure, one had it precipitated after performing a contrast-enhanced tomography scan and the other improved after discontinuation of tenofovir. Two remained on renal replacement therapy, one of them, without previous kidney disease, evolved with severe renal failure after COVID-19. At outcome no viral failure per protocol was documented, with 3 failures per ITT-E, all non-dialytic cases, two due to delay in ART withdrawal (albeit undetected in the last viral load) and one case changing to darunavir/r+dolutegravir+3TC triple regimen after viral load of 90 copies/mL
Lamivudine 150 mg/day was used in 12 cases, most cases with a high CD4+ T-cells count at diagnosis (503, IQR 35‒628 cells/mm3) and viral load of 13,065 (IQR 2971‒48,400 copies/mL). At the beginning of the 2DR, with a median age was 63 years old (IQR 53‒73), the CKD-EPI ranged from 3.80 to 55.80, with a median of 42 (IQR 28‒53). Time on ART was 633 weeks (IQR 309‒856), with suppression for 492 weeks (IQR 263‒868). 2DR use was monitored for 150 weeks (IQR 47‒165). Lamivudine 150 mg/day use ranged from 11 to 180 weeks (84, IQR 62‒161), with the maximum CKD-EPI ranging from 12.0 to 89.1 (35, IQR 24‒53) and minimum from 3.8 to 63.8 (29, IQR 6‒50). In the last available test, the CKD-EPI ranged from 26.4 to 68.0 (48, IQR 31‒66). At data censorship (April 7, 2022) 8/12 had adjusted the dose of 3TC to 300 mg/day. Three patients with CKD-EPI above 50 remained with 150 mg 3TC for 2‒25 weeks when dose was adjusted to 300 mg/day.
At week 48 on 2DR, 260/278 (93.5%) had a viral load assessment, and 257/260 (98.8%) was suppressed. Of those, 251/260 (96.5%) had no viral load detected (target not detected), 6/260 (2.3%) were below the assay limit, 50 copies/mL, with three detected (log10 of 2.5, 3.74 and 4.22). Considering missing tests as not suppressed, 92.4% (257/278) were suppressed below 50 copies/mL.
2DR was monitored for a median of 125 weeks (IQR 96‒170). Failure by ITT-E was documented in 19 cases; 8 for late withdrawal (greater than 30 days); 2 of these deaths due to cancer (suppressed in the last available test); 3 switched to triple therapy due to irregular monitoring and/or adherence; 2 for patient decision; 1 for two viral loads detected, but less than 200 copies/mL; 1 returned to triple therapy after changing service; 1 viremic since the beginning of ART, and 3 per-protocol failures.
In March 2022, 260 (93.5%) patients remained on regular use of 2DR, 249/260 (96%) 3TC+dolutegravir, 8 (3%) 3TC+darunavir/r and 3 (1%) 3TC+atazanavir/r. Additional 9 cases switching back to triple therapy, most to darunavir/r+dolutegravir+3TC. in two per-protocol failures, virological suppression was obtained after this triple therapy.
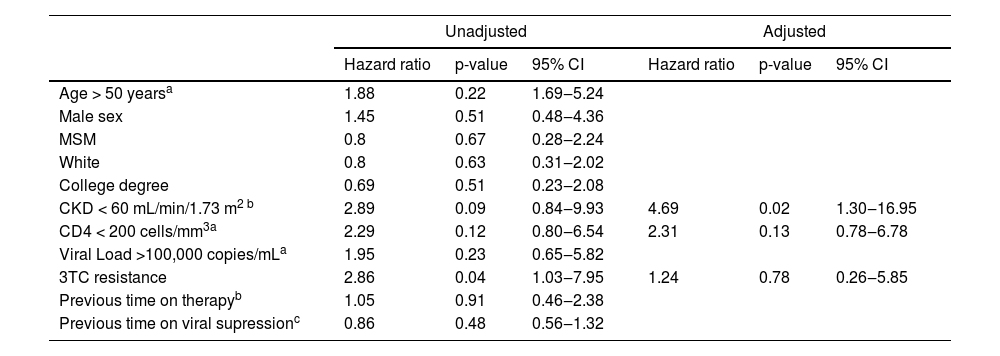
Outcomes are shown according to 3TC susceptibility in Table 3. To better evaluate the failure per-ITT-E, a Cox regression was used for demographic and laboratory variables, such as white, age at the start of 2DR, late diagnosis, and viral load < 100,000 copies/mL, with a p < 0.2 at unadjusted analyzes evaluated with adjusted analyses (Table 4), suggesting an independent role for a lower CKD in viral failure.
Cox regression model for the association of failure per Intent-To-Treat-Exposed (ITT-E).
95% CI, 95% Confidence Interval; MSM, Men who have Sex with Men; CKD, Chronic Kidney Disease Epidemiology Collaboration.
aAt admission.
bAt the initiation of 2DR, two-drug regimens.
cPeriod was considered from the first record of viral load < 50 copies/mL, for continuously period, without any result above 200 copies/mL during the period, up to start of 2DR.
Several studies have demonstrated the non-inferiority of the 2DR regimen compared to the triple ART regimen as a simplified therapy switch option for selected PLWH with virological suppression on triple ART,11,1316 as well as an initial therapeutic regimen for patients without pre-existing major viral resistance mutations to NRTIs, NNRTIs, or PIs.14 Our study documents similar suppression rates, comparable to other observational and clinical trials. The TANGO trial evaluated the efficacy and safety of switching to 3TC+dolutegravir (n = 369) vs. remaining on a Tenofovir Alafenamide (TAF)-based regimen (n = 372), demonstrated noninferiority of 2DR, with 93.2% in the 3TC+dolutegravir and 93% in the TAF-based regimen group with RNA < 50 copies/mL of HIV-1 at week 48. TANGO included adults PLWH with virologic suppression (HIV-1 RNA < 50 copies/mL) for > 6-months and taking a stable, first-line 3- or 4-drug TAF-based regimen (Tenofovir Disoproxil Fumarate, TDF to TAF switch ≥ 3-months before screening was allowed).13 In our study cases were included without these formal eligibility criteria, where the option to start or switch to 2DR, was made by the attending physician. One case started ART with 2DR and 9/278 previous virological suppression (HIV-1 RNA < 50 copies/mL) was inferior to 6-months. Even though, patients who remained using 2DR, 100% of 246 with samples collected at week 48 showed viral suppression (< 50 copies/mL) and 246/260 (94.6%) at the last observation. In comparison, the rate of suppression among all treated patients in the same service, with ART dispensed in the last 100 days of the year and who had performed a viral load in 2020, was 93% below 50 copies/mL, with rates of 89% reported for Brazil.17 Although the study cannot properly evaluate it, a better adherence profile might have influenced the practitioner's decision to suggest 2DR use. These favorable metrics are also suggested by other sub-analyses, as counting all cases, including cases without viral load available in week 48 in the denominator. In this case, 92.5% (257/278) reached virologic suppression (< 50 copies/mL), similar to the TANGO study.
We observed fewer suppression rates among those with presumed or documented 3TC resistance, not significantly different from those considered susceptible at Intention To Treat (ITT-E) analysis.
The Ministry of Health of Brazil in September 2021 recommended the use of 2DR for PLWH but established as criteria lack of 3TC resistance, in addition to clinical stability and virological suppression, ensuring that NRTI is fully active.18 All of our cases initiated 2DR previous to this recommendation, and some do not fully comply with current eligibility criteria. The European AIDS Clinical Society (EACS) Guideline19 refers to no historical resistance. Thus, lamivudine resistance would be considered an impediment to the use of 2DR as it could facilitate failure. However, some stable patients on long-term suppressive regimens even without fulfilling all criteria may benefit from 2DR. Rial-Crestelo et al. (2021) evaluated 21 cases after HIV-1 detection of RNA < 50 copies/mL for 1 year and maintained virological suppression at 96-weeks despite historical lamivudine resistance.20 Reynes et al. (2017), in the DOLULAM study, no participants experienced virologic failure (confirmed by HIV-1 detection of RNA ≥50 copies/mL) through week 104 among 27 with M184V/I mutation at the time of previous virologic failure in historical RNA genotypes.21 Galiardini et al. (2018) evaluated 436 patients starting lamivudine-based DR2, of which 87 (20%) did have the M184V mutation. Previous selection of M184V did not increase the risk of failure, however, in an additional analysis selecting patients with equal to or less than 3 years of viral suppression, the respective 1- and 3-year probabilities of remaining free from virological failure were 100.0% and 67.7% in the M184V+ group; and 97.3% and 96.2% in the M184V- group (p = 0.002).22 In our study, of 65 genotyped tests, only 13 were obtained during a 3TC failure, with 5 (38%) showing the M184V mutation. For our analysis, an additional 25 cases that had documented viremia above 200 copies/mL during 3TC use were inferred as also resistance to 3TC (group 3TC resistance). Failure was compared to those without evidence of resistance (3TC susceptible) per ITT-E (5/30 vs. 14/242, p = 0.044) and per protocol failure (1/30 vs. 1/242, p = 0.3). Results were similar when only inferred or documented resistance are considered (data not shown).
However, another point to take into consideration was the time on viral suppression before the start of 2DR, higher for the group 3TC resistance 532 (IQR 25%‒75% 219‒698) than 262-weeks (IQR 25%‒75% 107‒499) for 3TC susceptible (p = 0.003). It is likely that, as seen by Galiardini, the longer viral suppression time among lamivudine-resistant cases could contribute to sustained viral suppression. The time of follow-up in 2DR had a median of 125-weeks (IQR 25%‒75% 96‒170), similar to the 3TC resistance and 3TC susceptible group (p = 0.81) with similar success rates (viral load < 200 copies/mL in the last test using 2DR), 97% vs. 99% (p = 0.22).
In cases with renal dysfunction (CKD-EPI < 60 mL/min/1.73 m2), all 18 had viral load < 200 copies/mL in the last test using 2DR vs. 257/260 (99%) among cases without renal dysfunction (p = 0.65); however, had more failure per ITT-E, 17% vs. 6%, no significant difference in this limited cases numbers (p = 0.09). Only two cases of failure per protocol, without renal dysfunction (p = 0.71). However, our ITT-E analysis showed a significant association between failure with cases with CKD < 60 (p < 0.02). The Ministry of Health of Brazil restricted the use of dual therapy in cases with renal dysfunction that requires adjustment of the 3TC dose (CKD-EPI < 50 mL/min/1.73 m²), in September 2021.18 In our study, before this technical note, 12 cases had the 3TC dose adjusted to 150 mg/day, of which 4 underwent hemodialysis, at the beginning of the 2DR with a median of age 63 years old (IQR 25%‒75% 53‒73), from these, only one had its scheme modified after two viral loads of 90 copies/mL, despite only viral blips was considered failure per ITT-E due to therapy change. Tan et al. (2019) described 25 cases using 3TC+dolutegravir with an adjusted dose of 3TC and none experienced virological failure, suggesting that switching to dual therapy with 3TC and dolutegravir is well tolerated, durable and efficacious in this population with a median age of 60.5 years even on an adjusted of 3TC dose.23 Recently, it has been questioned whether there is a need to adjust the dose of 3TC for patients between 30 and 49 mL/min/1.73 m2.24 Whereas the use of 3TC (or another drug) is necessary with dolutegravir since monotherapy has shown higher rates of failure,25 the dose of 3TC may need to be adapted in some situations, as CKD-EPI < 50 mL/min/1.73 m2. Lamivudine, abacavir, and emtricitabine have only rarely been associated with lactic acidosis.26 The EACS Guidelines recommended dose adjustment of 3TC for impaired renal function to 150 mg if CKD-EPI 30‒49 mL/min, 100 mg if CKD-EPI 10‒29 mL/min, and 25–50 mg lamivudine daily to patients with CKD-EPI < 10 mL/min or undergoing hemodialysis.19 This issue is also unresolved, but in our study, of 12 with adjusted doses, no failure per protocol was observed. There are many limitations in our study, such as the limited number HIV resistance genotyping. Our retrospective study selected cases from the electronic medication dispensing system and the actual medication compliance was not documented. Although almost all using 2DR are included, the sample size does not have the power to properly address many issues as the different regimens used. This observational study lacked standardized criteria for the introduction and choice of 2 DR combination used.
Our study documents the effectiveness of switching to 2DR in our service as recommended today. Moreover, also suggests benefits for individuals not fulfilling all current requirements. Especially for these cases, close monitoring, and early intervention, when warranted, may allow 2DR use and still safeguard proper long-term virological suppression.
Transparency declarationsEMM reports personal fees from Abbott, Gilead, GSK-Viiv, Janssen, and Pfizer for consulting unrelated to the submitted work. The remaining authors declare that there are no conflicts of interest.