Globally HIV is the seventh leading cause of death among infants and children from 1 to 59 months of age. An estimated 230,000 children died from AIDS-related illnesses in 2011.1 Brazil has a mixed HIV epidemic, and pediatric cases are more common in the nine provinces of the north and northeast and survival after AIDS diagnosis is lower than in the rest of the country.2 The probability of survival at 60 months rose from 25% before 1988 to 88% in 2001–2002.3
To identify if the general improvement in survival was also extended to children in the Northeast region, we studied mortality in children with HIV infection in the state of Sergipe. A historical cohort of 101 HIV-infected children diagnosed from 1993 to 2011 was identified laboratory and surveillance databases, as well as from ambulatory medical records of the University Hospital and reference center. The starting date corresponds to the diagnosis of the first case of HIV in infants reported in Sergipe.
We examined two outcome variables. The first was death, and the second was survival from birth, as a proxy for survival time from HIV infection. We chose not to examine survival from AIDS diagnosis to death because a substantial proportion of cases were diagnosed close to death or post-mortem. For children who had not died, the date of censoring was the last record time of contact with the medical center. We used logistic regression analysis and a purposeful covariate selection process to identify predictors associated with death. Using the Wald, we further explored the variables in a multivariate analysis using stepwise modeling techniques. We removed covariates if statistical significance was lost (p-value<0.10) and the variable was found not to be a cofounder through its effect on other parameters in the models. Additionally, we performed a Kaplan–Meier survival analysis from birth, censoring data at death or last known day of follow-up. We conducted all analyses with the R 2.15.3 for Windows (R Development Core Team, Vienna, Austria). At the time we interviewed parents to complete data collection, we obtained informed consent. The study was approved by local ethical committee.
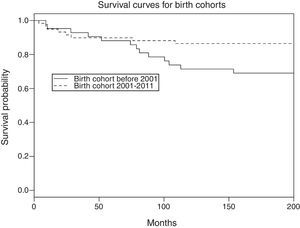
Between 1990 and 2011, 101 infants and children were diagnosed with HIV infection in Sergipe. Sixty-two (61%) were female, and the median age at HIV diagnosis was 3.0 years (interquartile range [IQR], 1.5–5.6 years). Twenty-one (21%) died. The median age at death was 4.3 years (IQR, 1.5–5.6 years). Nine (43%) children who had died were diagnosed with AIDS in their final hospital admission or post mortem, and four (19%) were diagnosed within four weeks of death. The median survival time from birth was 52 months (IQR, 18–88 months). Clinical factors associated with death in univariate analysis were the presence of clinical AIDS symptoms, CDC stage C disease, being born in 2000 or earlier and having a history of hospital admission. Being treated with triple-drug combination ART was protective. In a subset of patients for whom full records were available, antiretroviral prophylaxis, mode of delivery and avoidance of breastfeeding were not associated with death. In multivariate analysis, after adjusting for current treatment, the risk of death was 57% lower for children born after 2000 compared to those born≤2000 (adjusted relative risk [aRR] 0.43, p<0.05). Similarly, after adjusting for birth cohort, the risk of death decreased by 44% for every incremental advancement in treatment from no treatment to monotherapy to dual therapy to triple therapy (aRR 0.56, p<0.01). Lastly, the hazard ratio for death for children born after 2000 compared to those born≤2000 was marginally reduced (HR=0.42; p value=0.054) (Fig. 1).
We found that the risk of death decreased over time in children with HIV infection in the northeastern Brazilian state of Sergipe, consistently with trends seen in other settings around the world4,5 and in Brazil.3 Not surprisingly, sicker children, those with later stage disease, clinical AIDS and with histories of hospital admission, and those who had been inadequately treated were more likely to have died, as has been seen elsewhere.4,5 As HIV diagnosis becomes more timely in Brazil with near universal screening of pregnant women and early HIV antigen testing, we expect the proportion of children lately diagnosed to decrease and survival to rise.
We conclude that in this population-based registry study the risk of death is lower in children born after 2000 and is consistent with increasing survival that has been observed elsewhere in Brazil.3 As diagnosis of HIV becomes more timely with virologic testing of younger children, survival from HIV diagnosis to death will be an important indicator to monitor the quality of care in this population.
Conflicts of interestThe authors declare no conflicts of interest.
The authors wish to thank the health services for facilitating data collection and especially the students who assisted us in data collection: Gabriella Sousa Duarte, Nágyla Galvão Regis Martins, Deisiane Santana dos Santos, Cássia Barbosa da Silva.