The chronic hepatitis C (CHC) treatment is currently based on the use of direct-acting antivirals (DAAs), and patients infected with hepatitis C virus genotype 3 (GT3) have emerged as a more difficult-to-cure population. The NS5A inhibitor daclatasvir (DCV) and sofosbuvir (SOF), an NS5B viral polymerase inhibitor, are among the drugs that compose more effective and safer treatment regimens. The virus genetic variability is related to resistance-associated substitutions (RASs) that adversely impact DAAs effectiveness. The aims of this study were to analyze the association of NS5A and NS5B RASs and other clinical factors with DAAs regimens effectiveness in patients with GT3 CHC infection. This was a prospective cohort study performed in a Brazilian university hospital. Individuals older than 18 years with GT3 CHC treated with SOF + DCV ± ribavirin (RBV) or SOF + peginterferon (PEG) + RBV were included. Blood samples were collected at baseline and post-treatment. A total of 121 patients were included. Sustained virological response rates were 87.6% for the SOF + DCV ± RBV group and 80.0% for the SOF + PEG + RBV arm. Cirrhosis, prior treatment with interferon/PEG + RBV, and baseline NS5A RAS were associated with higher risk of treatment failure. The NS5A analysis suggested that A30K, Y93H, and RAS at site 62 were related to failure. Interestingly, a likely compensatory effect was shown between A30K and A62T. Emergence of Y93H was always associated with RAS at position 62. The RASs dynamics comprehension is an important tool to indicate more effective treatment for GT3 patients.
According to the World Health Organization, chronic hepatitis C infection (CHC) affects approximately 71 million people worldwide, causing 400,000 deaths every year due to complications such as cirrhosis, and hepatocellular carcinoma (HCC).1,2 In Brazil, it is estimated that 700,000 people are chronically infected with the hepatitis C virus (HCV).3 Regarding viral genotypes (GT), GT1 is the most prevalent, representing 44% of worldwide infections, followed by GT3 (25%) and GT4 (15%).2
The sustained virological response (SVR) promotes liver inflammation improvement, fibrosis regression, and liver-related mortality risk reduction.4 Advances in the virology field have provided a better understanding on HCV life cycle, allowing the development of direct acting antivirals (DAAs).5 In 2014, new DAAs were approved in the US, representing the beginning of a landscape that allowed the indication of drug combinations without interferon (INF) related to over 90% of SVR, and lower incidence of adverse drug reactions (ADRs) (INF-free era).6 The pangenotypic agents sofosbuvir (SOF), which acts as a nucleotide analogue inhibitor of NS5B RNA polymerase, and daclatasvir (DCV), which is an NS5A inhibitor, are among these drugs.7–10
The high replication rate and the lack of proofreading activity of the RNA-dependent RNA polymerase NS5B provide substantial genetic variability and an important HCV feature: the ability to circulate in the host as quasispecies.11,12 The variability is related to emergence of resistance-associated substitutions (RASs) that adversely impact DAAs effectiveness in vitro and/or in vivo.11,13,14 Usually these RASs are developed through selective pressure imposed by drugs that change the quasispecies population.15,16 However, mutations may naturally occur at baseline.14
Studies suggest that the impact of NS5A RASs in response to therapy would be higher when considering individuals with cirrhosis infected by GT3,5,17,18 and that infection by HCV GT3 is related to a higher risk of complications.19,20 Patients with GT3 CHC have emerged as a more difficult-to-cure population in the DAAs era.4,9,21
The RASs comprising amino acids 24 to 93 in NS5A and S282T mutation in NS5B are DAA-resistant substitutions commonly described in the literature.4 The aims of this study were to describe the prevalence of RASs in NS5A and NS5B at baseline and post-treatment in GT3 patients selected to receive DAAs, and to analyze the association of baseline and post-treatment RASs, besides other clinical factors, with DAA therapy effectiveness.
Material and methodsStudy setting and ethical aspectsThis was a real-life prospective cohort study performed at the University Hospital of the Ribeirão Preto Medical School, University of São Paulo, Brazil, a tertiary teaching institution linked to the Brazilian public health system. All molecular experiments and analysis were conducted at the Genomic Studies Laboratory of the São Paulo State University. The local ethics committee (research ethics committee of University Hospital) approved the design of this study (approval number 3,151,390), and written informed consent was obtained from all patients. The study was conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Patients and treatment regimensAll individuals older than 18 years with GT3 CHC receiving treatment from January 2016 to January 2020 were included. The treatment regimen indicated for each patient was based on the guidelines established for the Brazilian public health system (PCDT – Clinical Protocol for the Treatment of Hepatitis C and Co-infections). These guidelines were updated periodically. The versions used during the study period were PCDT 2015, PCDT 2017, and PCDT 2018. Therefore, the treatment regimens available for GT3 during the study were SOF + DCV ± ribavirin (RBV) for 12 weeks; SOF + DCV ± RBV for 24 weeks; or SOF + RBV + pegylated INF (PEG) for 12 weeks. According to these recommendations, the patients included in the study could be to be divided into two groups: SOF + DCV ± RBV and SOF + PEG + RBV. RBV was added to the SOF + DCV regimen used in all cirrhotic and non-cirrhotic patients who presented characteristics related to a lower probability of virological cure. In addition, the decision to include patients from both groups (SOF+DCV±RBV or SOF+PEG+RBV) was based on the objective to study both regions (NS5A and NS5B).10,22,23
Patients coinfected with human immunodeficiency virus infection and/or hepatitis B virus were not included. Individuals who were treated with two studied drug combinations in this research at different times were analyzed as different patients.
Clinical data collectionClinical and laboratory data were collected through access to the hospital computerized system. Regarding characterization of the study population in the pre-treatment period, the following information were collected: demographic data (age, sex, race/ethnicity), anthropometric data (weight and height), as well as clinical information concerning systemic arterial hypertension, diabetes mellitus, dyslipidemia, dialysis, liver fibrosis staging, hepatic encephalopathy, ascites, gastroesophageal varices, splenomegaly, prior treatment with INF/PEG + RBV, prior treatment with DAA, history of HCC, hepatic steatosis, treatment duration, use of RBV, and RASs. The results of the following laboratory tests performed at baseline were recorded: alanine aminotransferase, aspartate aminotransferase, albumin, serum bilirubins, international normalized ratio, platelets, creatinine, and HCV viral load. The Child-Turcotte-Pugh score to establish cirrhosis staging and MELD (model for end-stage liver disease) score were calculated considering exams undertaken up to six months before therapy.
The liver fibrosis staging was determined by biopsy (METAVIR classification) or liver elastography. Patients with hepatic encephalopathy, gastroesophageal varices, ascites and/or splenomegaly were clinically classified as cirrhotic.
HCV viral load quantification was performed 12 weeks after the end of treatment for patients treated with SOF and DCV. Regarding regimen involving PEG, the treatment response was verified at 12 and 24 weeks after therapy completion. HCV viral load was assessed by reverse transcription-polymerase chain reaction (RT-PCR), Abbott RealTime HCV assay, considering limit of detection < 12 UI/mL. SVR, relapsing, death and non-SVR due to early treatment discontinuation related to ADR were considered the study outcomes.
Resistance associated substitutions analysisGenome regions analyzed by groupNS5B was analyzed in all samples since both groups were treated with SOF, while NS5A was investigated only in those patients included in the group treated with DCV.
Collection of blood samplesRegarding the pre-treatment analysis, biological material was collected from all patients who went to the hospital up to 15 days before treatment and who consented to the procedure. For patients who completed the indicated treatment and did not achieve SVR, blood samples were collected at 12 and 24 weeks post-therapy. Sample collection was performed within 15 days after the date on which each individual completed 12 and 24 weeks post-treatment. For tests, about 8 mL of blood was collected in an 8.5 mL vacutainer tube with clot activator on its wall. After centrifugation, two 2 ml serum samples were separated and stored at -80°C.
RNA extraction and viral targets amplificationViral RNA extraction was performed using TRIzol. For each sample, 250 µl of serum were added to 750 µl of TRIzol (Thermo Fisher Scientific) followed by homogenization and incubation at room temperature for 5 min. Following the manufacturer's protocol, RNA was separated, precipitated and eluted in nuclease-free water. At this point, RNA was used as template for cDNA synthesis using the High Capacity cDNA Archive Kit (Life Technologies) according to the manufacturer's guidance protocol. After cDNA synthesis, viral targets NS5A and NS5B were amplified by the Nested Polymerase Chain Reaction (Nested-PCR) technique using the Long PCR Enzyme Mix (Thermo Fisher Scientific) following the manufacturer's instructions. For NS5B, the entire gene was amplified since RASs are found across the entire protein, and specific primers were designed for this process (Supplementary Table 1). For NS5A, primers from the literature were used to amplify the first 300 nucleotides since NS5A RASs are restricted to the domain I.24
Sanger sequencing and RAS frequency analysisAfter amplifications, the PCR products were submitted to the sequencing reaction using the BigDye Terminator v3.1 (Life Technologies). For NS5A, the primers for the second PCR reaction were used for sequencing, while for NS5B, besides the internal Nested-PCR primers, an additional pair of internal primers were used to sequence the whole fragment (Supplementary Table 2).
The sequencing was performed using an ABI 3130 XL Genetic Analyzer (Life Technologies) and the obtained sequences were aligned by Clustal W nested in the BioEdit 7.1.11 package.25,26 The RASs occurrence analysis was performed by the comparison of the sequences with the reference sequence for GT3 - NZL1 (GeneBank accession number D17763).
Statistical analysisThe quantitative variables age and pre-treatment viral load were described as mean and standard deviation. Other variables were categorized and their absolute and relative frequencies are reported. The global SVR rate and SVR rates according to treatment regimens were determined by intention-to-treat. The association analysis between clinical variables and the SVR for each study arm, in addition to analysis between the treatment regimen used and SVR, were assessed with relative risks (RR) calculated by log-binomial model.
Log-binomial regression was performed for each group to verify which clinical variables would be more strongly associated with SVR. The variables whose analysis presented p < 0.05 from crude RR were considered for the regression model. For all association analyses a 5% significance level (α) was established, and the tests were performed using the Statistical Package for Social Sciences software (SPSS Inc., Version 21.0).
ResultsPatient characteristicsA total of 121 patients chronically infected by HCV GT3 were included in the study, 82 (67.8%) of whom were men. The average age was 56.4 ± 8.5 years and 93 (76.9%) patients had cirrhosis. Among those with cirrhosis, this condition was diagnosed by biopsy in 15 patients (16.1%), by elastography in 28 patients (30.1%), by clinical evaluation in 50 patients (53.8%); 76 individuals (81.7%) presented compensated liver disease. Regarding the treatment regimens, 105 (86.8%) individuals were treated with SOF + DCV ± RBV, 15 (12.4%) used SOF + PEG + RBV, and one patient (0.8%) was treated with SOF + DCV + PEG + RBV. All demographic and clinical data are described in Table 1.
Baseline demographic and clinical characteristics of GT3 CHC patients treated with antiviral therapy.
| Characteristics | All patients(n = 121)* | SOF + DCV ± RBV(n = 105) | SOF + PEG + RBV(n = 15) |
|---|---|---|---|
| Age (years), mean (SD) | 56.4 (8.5) | 56.8 (8.3) | 53.1 (9.2) |
| Male, n (%) | 82 (67.8) | 68 (64.8) | 13 (86.7) |
| Race/Ethnicity, n (%) | |||
| White | 104 (86.0) | 89 (84.8) | 14 (93.3) |
| Other | 17 (14.0) | 16 (15.2) | 1 (6.7) |
| Diabetes Mellitus, n (%) | 35 (28.9) | 30 (28.6) | 4 (26.7) |
| Hypertension, n (%) | 50 (41.3) | 44 (41.9) | 6 (40.0) |
| Obesity, n (%) | 36 (29.8) | 32 (30.5) | 3 (20.0) |
| Dyslipidemia, n (%) | 26 (21.5) | 22 (21.0) | 4 (26.7) |
| Liver fibrosis stage, n (%) | |||
| F0/F1 | 6 (5.0) | 5 (4.8) | 1 (6.7) |
| F2 | 10 (8.3) | 9 (8.6) | 1 (6.7) |
| F3 | 12 (9.9) | 8 (7.6) | 4 (26.7) |
| F4 | 93 (76.9) | 83 (79.0) | 9 (60.0) |
| Child-Turcotte-Pugh score, n (%)⁎⁎ | |||
| A | 76 (81.7) | 68 (81.9) | 8 (88.9) |
| B | 13 (14.0) | 12 (14.5) | 1 (11.1) |
| C | 2 (2.2) | 2 (2.4) | 0 (0.0) |
| MELD score, n (%)⁎⁎ | |||
| ≤ 9 | 50 (53.8) | 44 (53.0) | 6 (66.7) |
| 10-19 | 37 (39.8) | 34 (41.0) | 3 (33.3) |
| 20-29 | 4 (4.3) | 4 (4.8) | 0 (0.0) |
| HCV-RNA, mean x 106 UI/mL (SD) | 1.1 (1.2) | 1.1 (1.3) | 1.1 (0.9) |
| AST ≥ 3x ULN, n (%) | 36 (29.8) | 32 (30.5) | 4 (26.7) |
| ALT ≥ 3x ULN, n (%) | 41 (33.9) | 36 (34.3) | 4 (26.7) |
| Platelets < 100.000 mm3, n (%) | 41 (33.9) | 37 (35.2) | 3 (20.0) |
| History of HCC, n (%) | 13 (10.7) | 13 (12.4) | 0 (0.0) |
| Antiviral treatment history, n (%) | |||
| INF or PEG + RBV | 53 (43.8) | 43 (41.0) | 9 (60.0) |
| SOF | 3 (2.5) | 2 (1.9) | 0 (0.0) |
| DCV + SOF | 2 (1.7) | 2 (1.9) | 0 (0.0) |
| Treatment duration, n (%) | |||
| 12 weeks | 94 (77.7) | 79 (75.2) | 15 (100.0) |
| 24 weeks | 27 (22.3) | 26 (24.8) | 0 (0.0) |
| Use of RBV, n (%) | 106 (87.6) | 90 (85.7) | 15 (100.0) |
| eGFR (CKD-EPI equation), n (%) | |||
| G1 (> 90 ml/min/1.73m2) | 61 (50.4) | 49 (46.7) | 11 (73.3) |
| G2 (60-89 ml/min/1.73m2) | 43 (35.5) | 40 (38.1) | 3 (20.0) |
| G3a (45-59 ml/min/1.73m2) | 5 (4.1) | 4 (3.8) | 1 (6.7) |
| G3b (30-44 ml/min/1.73m2) | 7 (5.8) | 7 (6.7) | 0 (0.0) |
| G4 (15-29 ml/min/1.73m2) | 2 (1.7) | 2 (1.9) | 0 (0.0) |
| G5 (< 15 ml/min/1.73m2) | 3 (2.5) | 3 (2.9) | 0 (0.0) |
| Hepatic steatosis, n (%) | 39 (32.2) | 33 (31.4) | 5 (33.3) |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; CHC, chronic hepatitis C; CKD-EPI, chronic kidney disease epidemiology collaboration; DCV, daclatasvir; eGFR, estimated glomerular filtration rate; GT3, genotype 3; HCC, hepatocellular carcinoma; INF, interferon; MELD, model for end-stage liver disease; Obesity, body mass index ≥ 30.0 Kg/m2; PEG, pegylated interferon; RBV, ribavirin; SD, standard deviation; SOF, sofosbuvir; ULN, upper limit of normal.
Regarding NS5A protein, 94 samples (79 pre- and 15 post-treatment) were collected with 92.6% amplification efficiency (NS5A amplified from 87 samples). For NS5B, 106 samples (91 pre- and 15 post-therapy) were considered with 80.2% amplification success rate (NS5B amplified from 85 samples).
The frequency analysis of baseline RASs, calculated from amplified samples, showed that the most prevalent site for RASs in NS5A was position 62 (63.3% of individuals treated with SOF + DCV ± RBV presented RAS A62S and 24.1% presented A62T). For NS5B, position G554A was the most prevalent RAS (3.7% considering all samples amplified for this region at baseline). All NS5B mutations (baseline and post-treatment) were detected in the SOF + DCV ± RBV arm. The prevalence of all baseline RASs in this group are shown in Table 2.
Baseline-resistance associated substitutions in the SOF + DCV ± RBV group.
| NS5A (n = 79)* | NS5B (n = 70)* | ||
|---|---|---|---|
| RAS | n (%) | RAS | n (%) |
| M28 | 0 (0.0) | L159F | 1 (1.4) |
| P29 | 0 (0.0) | S282 | 0 (0.0) |
| A30K | 6 (7.6) | C316 | 0 (0.0) |
| A30T | 2 (2.5) | V321 | 0 (0.0) |
| A30S | 1 (1.3) | S368 | 0 (0.0) |
| L31 | 0 (0.0) | N411 | 0 (0.0) |
| P32 | 0 (0.0) | M414 | 0 (0.0) |
| P58T | 1 (1.3) | V421A | 1 (1.4) |
| A62F | 2 (2.5) | Y448 | 0 (0.0) |
| A62I | 1 (1.3) | P495 | 0 (0.0) |
| A62L | 1 (1.3) | V553 | 0 (0.0) |
| A62T | 19 (24.1) | G554A | 3 (4.3) |
| A62S | 50 (63.3) | G556 | 0 (0.0) |
| E92D | 1 (1.3) | D559 | 0 (0.0) |
| Y93 | 0 (0.0) | ||
RAS, resistance associated substitution.
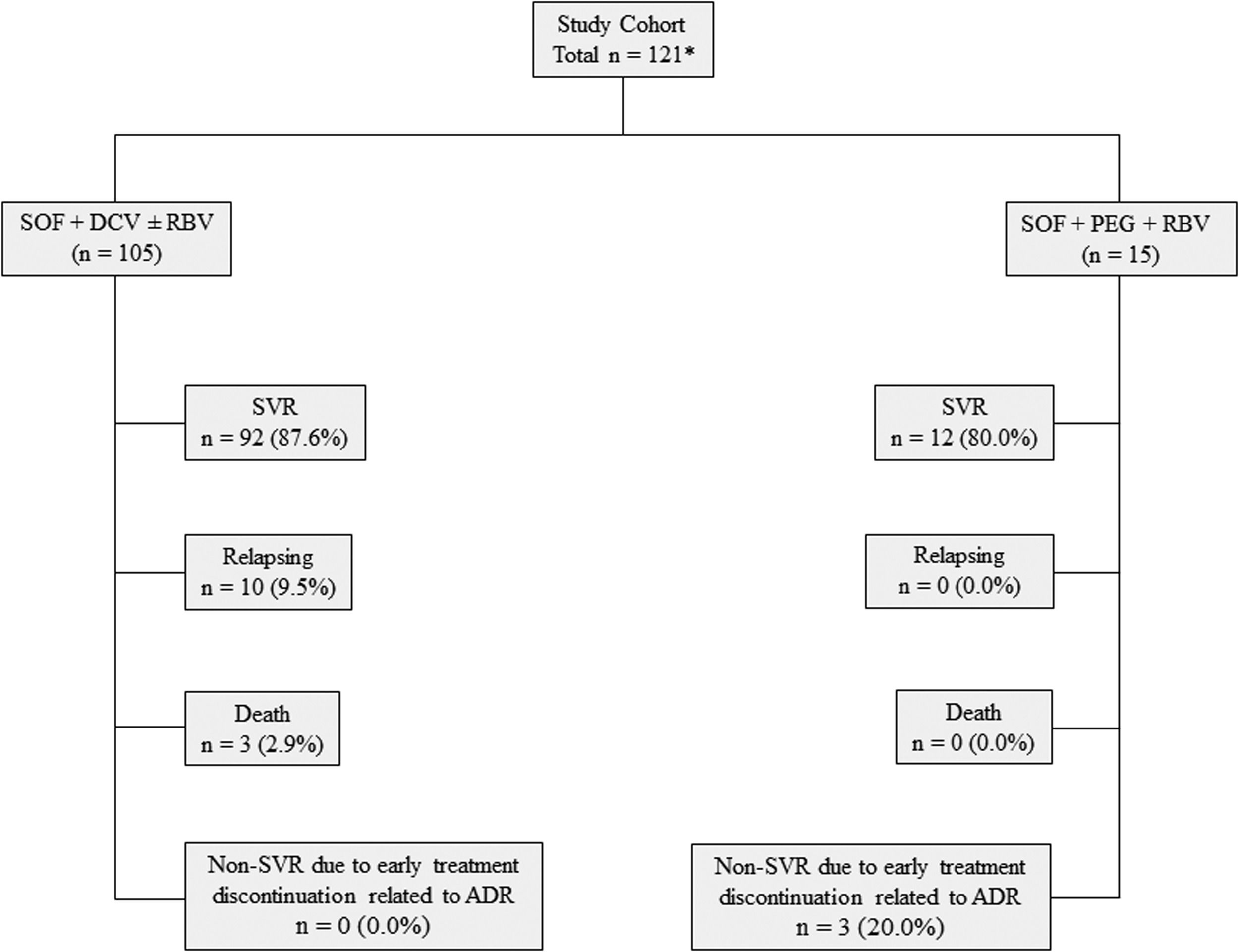
SVR rates were 86% for the general study population, 87.6% for the SOF + DCV ± RBV group, and 80% for the SOF + PEG + RBV arm. The treatment response analysis, considering patients with available response data, indicated SVR rates of 88.1% for the general study population and 90.2% for the SOF + DCV ± RBV group. Regarding the SOF + PEG + RBV group, the SVR rate was 100% when evaluating individuals who had completed treatment. The treatment outcomes of all patients treated with SOF + DCV ± RBV or SOF + PEG + RBV are described in Fig. 1.
The patient who used SOF + DCV + PEG + RBV for 24 weeks presented treatment relapse. The three individuals who died during treatment had cirrhosis, two of them had decompensated liver disease. The comparison of SVR rates showed that patients in the two treatment arms (SOF + DCV ± RBV x SOF + PEG + RBV) were equally likely to achieve SVR (RR = 1.128; CI 95% = 0.869-1.464).
Factors associated with SVROverall, 14 patients relapsed, presenting detectable HCV RNA at 12 or 24 weeks after treatment. Data for the association analysis between clinical variables and SVR and the SVR rates according to each variable are described in Table 3.
SVR rates according to clinical variable subgroups and association analysis of these variables with SVR in the different treatment groups.
| All patients* | SOF + DCV ± RBV | SOF + PEG + RBV | ||||
|---|---|---|---|---|---|---|
| SVR (%) | RR | SVR (%) | RR | SVR (%) | RR | |
| (95% CI) | (95% CI) | (95% CI) | ||||
| Cirrhosis | 1.184 (1.084-1.294) | 1.143 (1.052-1.242) | 1.500 (0.945-2.381) | |||
| No cirrhosis | 100.0 | 100.0 | 100.0 | |||
| Cirrhosis | 84.4 | 87.5 | 66.7 | |||
| Cirrhosis stage⁎⁎ | 1.009 (0.785-1.295) | 1.057 (0.808-1.381) | 0.625 (0.365-1.069) | |||
| Compensated | 85.3 | 88.1 | 62.5 | |||
| Decompensated | 84.6 | 83.3 | 100.0 | |||
| Diabetes Mellitus | 1.040 (0.891-1.214) | 1.003 (0.871-1.155) | 1.091 (0.581-2.050) | |||
| No | 89.2 | 90.3 | 81.8 | |||
| Yes | 85.7 | 90.0 | 75.0 | |||
| CKD stage⁎⁎⁎ | 0.966 (0.791-1.180) | 0.991 (0.812-1.209) | — | |||
| Non-severe CKD | 87.9 | 90.1 | 80.0 | |||
| Severe CKD | 90.9 | 90.9 | — | |||
| Treatment duration | NA | 0.984 (0.850-1.139) | NA | |||
| 12 weeks | NA | 89.9 | 80.0 | |||
| 24 weeks | NA | 91.3 | NA | |||
| Use of RBV | NA | 1.034 (0.880-1.216) | NA | |||
| No | NA | 92.9 | NA | |||
| Yes | NA | 89.8 | 80.0 | |||
| Previous therapy with INF/PEG + RBV | 1.157 (1.002-1.336) | 1.134 (0.981-1.310) | 1.071 (0.650-1.767) | |||
| No | 93.9 | 94.9 | 83.3 | |||
| Yes | 81.1 | 83.7 | 77.8 | |||
| Baseline RAS⁎⁎⁎⁎ | ||||||
| NS5A RAS | NA | 1.125 (1.037-1.221) | NA | |||
| No | NA | 100.0 | NA | |||
| Yes | NA | 88.9 | NA | |||
| A62T (NS5A RAS) | NA | 1.200 (0.929-1.550) | NA | |||
| No | NA | 93.3 | NA | |||
| Yes | NA | 77.8 | NA | |||
| A62S (NS5A RAS) | NA | 0.932 (0.785-1.106) | NA | |||
| No | NA | 85.7 | NA | |||
| Yes | NA | 92.0 | NA | |||
| NS5B RAS | 1.133 (0.727-1.767) | 1.152 (0.739-1.797) | — | |||
| No | 90.7 | 92.2 | 81.8 | |||
| Yes | 80.0 | 80.0 | — | |||
CI, confidence interval; CKD, chronic kidney disease; DCV, daclatasvir; INF, interferon; NA, not applied; PEG, pegylated interferon; RAS, resistance associated substitutions; RBV, ribavirin; RR, relative risk; SOF, sofosbuvir; SVR, sustained virologic response.
—: not calculated due to the absence of individuals in a subgroup of the analyzed variable.
Cirrhosis, history of previous treatment with INF/PEG + RBV, and presence of baseline RAS at NS5A viral protein were factors associated with a higher risk of treatment failure. Absence of cirrhosis was associated with SVR in the general study population (p = 0.034) and in the SOF + DCV ± RBV group (p = 0.023). The association between SVR and no previous treatment with INF/PEG + RBV was also observed in the general cohort (p = 0.026), while the analysis of the SOF + DCV ± RBV group showed that treatment failure was associated with the presence of baseline RAS in NS5A (p = 0.028). Regarding the general group, the log-binomial regression model adjusted for the variables cirrhosis and history of previous treatment with INF/PEG + RBV showed that previous treatment with INF/PEG + RBV was the clinical variable more strongly associated with the treatment failure (p = 0.030; adjusted RR = 3.85; 95% IC = 1.13-7.32). The small number of the patients of the studied variables subgroups with p < 0.05 in the SOF + DCV ± RBV arm did not allow to perform regression analysis.
RASs and treatment responseThere was no relationship between isolated A62S (the most prevalent pre-treatment RAS) and treatment failure. About A62T RAS, although no statistical relevance was observed, the results suggest a 20% higher chance to achieve SVR (RR = 1.200; CI 95% = 0.929-1.550) in patients who did not present this RAS at baseline (Table 3). The NS5A RAS A30K was detected in six samples, always associated with another mutation at position 62. All patients with viral variants that carried both A30K and A62T mutations failed the treatment. These patients presented A30K + A62T in pre-treatment and maintained the mutations at post-failure. In contrast, those individuals whose samples presented A30K and A62S achieved SVR.
Regarding RASs detected at post-treatment in blood samples from patients who completed drug therapy and did not achieve SVR, the NS5A RAS Y93H was detected in four of these samples. All of these individuals concomitantly presented a mutation at site 62. However, Y93H was not observed in pre-treatment samples. Two patients were treated with SOF + DCV + RBV for 12 weeks and retreated with the same regimen for 24 weeks. In one of them who presented A30K and A62T, the E92D mutation after the pressure of the first treatment was detected. The presence of these three RASs was also a feature of baseline retreatment indicated six months after first therapy completion. The Y93H and A62T were detected after therapy with SOF + DCV + RBV for 12 weeks in the other patient. The same individual presented A62T in NS5A before retreatment for 24 weeks performed three years later.
Concerning NS5B, L159F was the only RAS detected after DAA use. It was observed in a single relapsing patient in pre- and post-treatment samples. Demographic and clinical data of all patients included in the study who did not achieve SVR are described in Table 4.
Demographic and clinical characteristics of GT3 CHC patients who did not achieve SVR.
| Case | Age | Sex | Cirrhosis | INF/PEG + RBV treatment history | DAA treatment history | Drugs used in the study | Therapy duration | Pre-therapy RAS NS5A | Pre-therapy RAS NS5B | Post-therapy RAS NS5A | Post-therapy RAS NS5B |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 42 | F | Yes | Yes | No | SOF+DCV+ RBV | 12 W | A62S | — | A62SY93H | — |
| 2 | 48 | M | Yes | Yes | No | SOF+DCV+ RBV | 12 W | A62S | L159F | A62SY93H | L159F |
| 3 | 67 | M | Yes | Yes | No | SOF+PEG+ RBV | 5 days* | NA | — | NA | NA |
| 4 | 66 | M | Yes | No | No | SOF+DCV | 12 W | A30KA62T | None | A30K A62T | — |
| 5 | 62 | M | Yes | Yes | No | SOF+DCV+ RBV | 12 W | A62S | — | A62SY93H | — |
| 6 | 56 | F | Yes | No | No | SOF+DCV+ RBV | 12 W | A62S | None | — | — |
| 7 | 55 | M | Yes | No | No | SOF+DCV+ RBV | 12 W | — | — | — | — |
| 8 | 62 | M | Yes | Yes | SOF | SOF+DCV+ PEG+RBV | 24 W | — | — | A62T | — |
| 9 | 51 | F | Yes | No | No | SOF+PEG+RBV | 2 W* | NA | None | NA | NA |
| 10 | 62 | M | Yes | Yes | No | SOF+PEG+RBV | 3 W* | NA | None | NA | NA |
| 11 | 49 | M | Yes | Yes | No | SOF+DCV+RBV | 12 W | A30KA62T | None | A30KA62TE92D | None |
| 12 | 50 | M | Yes | Yes | SOF + DCV | SOF+DCV+RBV | 24 W | A30KA62TE92D | None | A30KA62T | None |
| 13 | 54 | M | Yes | Yes | No | SOF+DCV+RBV | 12 W | — | — | A62TY93H | None |
| 14 | 57 | M | Yes | Yes | SOF + DCV | SOF+DCV+RBV | 24 W | A62T | None | — | — |
CHC, chronic hepatitis C; DAA, direct acting antiviral; DCV, daclatasvir; GT3, genotype 3; INF, interferon; NA, not applied; PEG, pegylated interferon; RAS, resistance associated substitution; RBV, ribavirin; SOF, sofosbuvir; SVR, sustained virologic response.
—: blood sample not collected or not amplified.
Participants of this study had a high prevalence of cirrhosis (76.9%). Although individuals with GT3 CHC have a higher risk of developing cirrhosis, this finding is also related to the treatment criteria of the Brazilian guidelines. Until 2018, patients without fibrosis (F0) or with mild fibrosis (F1) who had no other specific clinical conditions established in the treatment protocol were not eligible for treatment with DAAs.10,22
No significant difference in SVR rates was observed when comparing groups treated with SOF + DCV ± RBV or SOF + PEG + RBV. This result corroborates the findings of studies that showed similar effectiveness between these treatment regimens.17,27–29 The use of SOF + PEG + RBV for GT3 was recommended based on data that showed SVR rates close to 90%.27,30 Despite high effectiveness (100% SVR among individuals who completed treatment), the indication of this treatment regimen was limited worldwide by the higher incidence of serious adverse events.
Cirrhosis, prior treatment with INF/PEG + RBV, and baseline NS5A RAS were variables associated with treatment failure. There was a higher risk of non-response among cirrhotic individuals considering all patients and the SOF + DCV ± RBV group according crude RR analysis. All non-responder patients included in the study had cirrhosis. The association between cirrhosis and non-SVR in individuals infected with HCV GT3 was shown by different studies that analyzed the effectiveness of SOF + DCV ± RBV, SOF + PEG + RBV and other drug combinations involving DAAs.17,28,29,31–33 As already mentioned, the treatment of GT3-infected cirrhotic patients is the main challenge of the DAAs era.
The association analysis between prior dual therapy with INF/PEG + RBV and SVR showed that INF/PEG + RBV-experienced patients have a higher risk of non-SVR when analyzing the general study population. Similar results were found in other real-life studies that included individuals chronically infected with GT3 treated with SOF + DCV ± RBV.8,34 The small number of DAA-experienced patients in our study did not allow statistical analysis between SVR and prior DAA treatment-experience.
The analysis of the SOF + DCV ± RBV group showed that the presence of RAS in NS5A at baseline was associated with treatment failure. All non-responders treated with SOF + DCV ± RBV presented at least one NS5A RAS in all amplified samples (baseline and post-treatment) and this finding corroborates the literature that indicates a high prevalence of NS5A mutations in non-responders to NS5A inhibitor regimens.35–37 The NS5A RASs have particular clinical relevance because NS5A inhibitors are part of all treatment combinations recommended in the main guidelines worldwide.3–5 In addition, RASs in this protein are usually maintained in the viral population due to a lower impact on viral fitness when compared to mutations in other genomic regions. Therefore, these mutations can persist for several years and impact the response to retreatment of patients with previous failure to the NS5A inhibitor. In general, substitutions in NS5B and NS3 proteins rapidly disappear from the viral population in post-failure.35
According to the European Association for the Study of the Liver, physicians who have access to reliable NS5A RAS testing at baseline (spanning 24 to 93 amino acids) should consider their results when making decisions regarding the choice of therapy.38 The same guideline recommends a population sequencing approach that was used in the present study.
Considering the most prevalent NS5A RASs at pre-treatment in the SOF + DCV ± RBV arm, A62S and A62T were found in 63.3% and 24.1% of the samples, respectively. No association was found between A62S mutation at baseline and SVR. However, our findings showed a higher baseline prevalence of A62T among non-responders. This RAS became the most prevalent RAS at site 62 in post-therapy, showing some sort of maintenance after selective pressure treatment. Although the association between mutations at position 62 and high levels of resistance in vitro is not described in the literature,35,39 these results suggest that the change for a threonine (T) could be related to non-SVR. One individual (patient 8, Table 4) was treated with SOF + DCV + PEG + RBV for 24 weeks and did not achieve SVR. This patient presented only A62T after therapy.
The impact of RASs in position 30 on failure to DAAs in different GTs is known and well described.4 Substitutions that exhibit resistance fold-change (FC) in vitro > 100 promote a very high level of resistance,37 and the A30K RAS confers an FC of 117 for DCV in GT3a, the most prevalent GT3 subtype in Brazil and worldwide.35,40 Our data showed that A30K was found in six patients at baseline always associated with a mutation at site 62 (A62T or A62S). Interestingly, only the clinical samples that presented A30K + A62T at baseline failed the treatment, showing a possible compensatory effect between these RASs and reinforcing the possible relation between A62T with treatment failure. In all cases, the two RASs were maintained in the post-treatment analyses.
Among the NS5A RASs, Y93H is described as the most related to failure to DCV or other NS5A inhibitors for GT3 and other GTs.14,17,18,35,40 The FC of Y93H in vitro for DCV in GT3a ranges from 2,154 to 3,733.14,35 In pre-treatment analysis, Y93H was not detected. However, after DCV selective pressure, Y93H was highly frequent in clinical samples of the relapsing patients. Despite lower impact that NS5A RASs promote on viral replication in relation to substitutions in other proteins, variants with Y93H may show defective viral fitness.41 In our population, Y93H was circulating in a lower frequency before treatment in the infected population and was not detected by the Sanger sequencing method. However, it became prevalent after DAA therapy. In this scenario, the change in host environment prompted by DCV selective pressure possibly benefitted variants bearing Y93H. In addition, in all samples from which Y93H was detected, a mutation at position 62 was also found (three with RAS A62S and one with RAS A62T). A recent study conducted by our group, showed that Y93H can act together with other NS5A substitutions enhancing resistance,42 while McPhee et al.43 analyzed samples of GT3a patients under DCV therapy and found that the presence of A62L with Y93H had a threefold increase of FC in relation to samples that presented only Y93H. Our results suggest that the association of RASs may be an important mechanism to mitigate the negative impact on viral fitness of some substitutions.
Another RAS found in non-responders was E92D. Despite the known relation of this site with DAAs resistance, there is no information regarding this specific substitution.14,18,35,39,40 Although the NS5A inhibitor evaluated in our study has been excluded from some developed countries guidelines, this drug is part of the treatment access strategies in several world regions specially in developing countries.44 In addition, cross-resistance among NS5A inhibitors is a characteristic of the class.14 Considering GT3a, Y93H is related to an FC of 724 to velpatasvir (VEL).14,35 Results from clinical trials suggest association between Y93H and A30K with response to VEL- or pibrentasvir-containing regimens.45,46
The same approach involving RASs was performed for NS5B and a low prevalence of mutations in the RNA-dependent RNA polymerase was observed. RAS S282T is the substitution that confers high resistance to SOF in vitro, however it was not detected in our samples. This finding corroborates the results of other clinical trials.47,48 The replicative capacity of viral variants that develop S282T is substantially reduced compared to the wild virus or variants without RAS in this site.49 In contrast, L159F was found in a non-responder individual (patient 2, Table 4). Observing the tertiary structure of the viral protein, L159F and S282 are only four angstrom distant from each other, and the interaction between them would lead to a change in the catalytic site conformation, influencing SOF activity.50
Although guidelines and real-life studies indicate that longer therapies (24 weeks) and use of RBV can mitigate the impact of RASs in patients with cirrhosis,5,8,9 the analysis of the SOF + DCV ± RBV group did not corroborate these strategies. The American guideline recommends adding RBV to the VEL + SOF regimen for 12 weeks for treatment-naive GT3 patients with compensated cirrhosis if the pre-treatment RAS testing detects Y93H.5 In the SOF + DCV ± RBV arm, a single non-responder patient who had chronic kidney disease (CKD stage = 4) and anemia prior to treatment did not use RBV. Regarding the persistence of NS5A RASs, a non-responder (patient 14, Table 4) had a history of previous treatment with NS5A and detection of Y93H at post-failure (patient 13, Table 4). Retreatment was performed three years after initial treatment failure which suggests that in less than three years the variants that contained this RAS became less prevalent.
Our study has limitations. One of the limitations was the small sample size. Notably, the number of non-cirrhotic patients. Therefore, the analysis of the impact of RASs on treatment response among non-cirrhotic individuals was limited. This is a real-life study in a public hospital. During the study period, treatment with DAAs was available in the Brazilian public health system mainly for patients with advanced liver fibrosis. It was not possible to collect or amplify blood samples from all patients at all points according to methods.
ConclusionsIn conclusion, this study suggests that NS5A RASs are associated with the failure of DCV treatment regimes in patients with GT3 CHC, including RASs at site 62. The detection of RASs combined with the comprehension of selection dynamics are important tools to indicate more effective treatment regimens in more difficult-to-cure populations.
Authors’ contributionsStudy conception and design: A.L.C. Martinelli, L.R.L. Pereira, P. Rahal, F.F. Souza. Acquisition of data: G.F.R. Campos, J.P.V. Rodrigues. Performing experiments: G.F.R. Campos, J.P.V. Rodrigues. Analysis and interpretation of data: All. Drafting of manuscript: G.F.R. Campos, J.P.V. Rodrigues. Critical revision: All. Supervision: A.L.C. Martinelli, L.R.L. Pereira, P. Rahal, F.F. Souza.
Financial supportThis work was funded by FAPESP – São Paulo Research Foundation (Scholarship Grants 2016/03807-0 and 2018/04678-5; Project Grant 2017/22927-0).