The aim of this study was to evaluate the impact of a bundle called FAST HUG in ventilator-associated pneumonia, weigh the healthcare costs of ventilator-associated pneumonia patients in the intensive care unit, and hospital mortality due to ventilator-associated pneumonia.
Material and methodsThe study was performed in a private hospital that has an 8-bed intensive care unit. It was divided into two phases: before implementing FAST HUG, from August 2011 to August 2012 and after the implementation of FAST HUG, from September 2012 to December 2013. An individual form for each patient in the study was filled out by using information taken electronically from the hospital medical records. The following data was obtained from each patient: age, gender, reason for hospitalization, use of three or more antibiotics, length of stay, intubation time, and outcome.
ResultsAfter the implementation of FAST HUG, there was an observable decrease in the occurrence of ventilator-associated pneumonia (p<0.01), as well as a reduction in mortality rates (p<0.01). In addition, the intervention resulted in a significant reduction in intensive care unit hospital costs (p<0.05).
ConclusionThe implementation of FAST HUG reduced the number of ventilator-associated pneumonia cases. Thus, decreasing costs, reducing mortality rates and length of stay, which therefore resulted in an improvement to the overall quality of care.
Ventilator-associated pneumonia (VAP) is the second most common health care-associated infections (HAI) in the United States and is responsible for 25–42% of all infections that occur in intensive care units (ICUs). Among those patients requiring mechanical ventilation, mortality rates are 46% in patients with VAP.1–3 Patients with VAP have significantly increases the length of hospital stay and thus healthcare costs. This however could be reduced if steps are taken to improve the care provided for the ventilated patient. Therefore, the prevention of VAP must be a priority in the care of critically ill patients.4–6
Health professionals continually strive to improve the care provided for patients admitted to ICU.3 The results of recent quality improvement initiatives suggest that many cases of VAP could be prevented by paying careful attention when delivering care, which is the primary role of the FAST HUG checklist. FAST HUG is a mnemonic aid to ICU healthcare professionals to prepare for patient rounds, help identify and prevent medication errors, promote patient safety, and maximize therapeutic interventions.3,7
In this study, we evaluate the impact of FAST HUG in the occurrence of VAP, weigh the healthcare costs of VAP patients in the ICU, and hospital mortality due to VAP.
Materials and methodsStudy designThe study was performed in a private hospital in the city of Uberlandia, Minas Gerais-Brazil that has an 8-bed ICU. It was divided into two phases: before implementing FAST HUG, from August 2011 to August 2012 and after the implementation of FAST HUG, from September 2012 to December 2013. The research was conducted after the approval of the Ethics Committee on Human Research of the Federal University of Uberlandia, according to the registry protocol CEP/UFU: 442.151/2013.
An individual form for each patient in the study was filled out by using information taken electronically from the hospital medical records. The following data was obtained from each patient: age, gender, reason for hospitalization, use of three or more antibiotics, length of stay, intubation time, and clinical outcome. Furthermore, the FAST HUG checklist, which corresponds to 10 items, was followed and printed out daily by the nursing staff.
The study inclusion criteria were age over 18 years, be hospitalized at the study hospital, and using a mechanical ventilator (MV) for over 48h.
DefinitionsFAST HUG is a checklist that highlights key aspects of general care for critically ill patients. The mnemonic aid stresses the importance of the following clinical practices: feeding, analgesia, sedation, thromboembolic prophylaxis, head of bed elevation, stress ulcer prophylaxis, and glycemic control. FAST HUG can be applied to all ICU patients.3 According to scientific literature, there are also three important actions to be taken in order to reduce VAP, which are: oral hygiene with 2% chlorhexidine, monitoring cuff pressure between 20 and 25cm of water, and subglottic suction every six hours or whenever necessary.2,3
VAP: mechanically ventilated patients whose condition has evolved to the point where a new or progressive pulmonary infiltrate in a chest X-ray. The definition also requires at least two clinical signs and/or laboratory abnormalities that suggest an infectious process such as: fever (>38°C); leukocytosis (>10,000mm–3) or leukopenia (<4000mm–3); presence of purulent tracheal secretion after 48h of ventilation.1,3,8
Statistical analysisThe Kolmogorov–Smirnov and Shapiro–Wilk tests were used to test the normality of all the variables. The Mann–Whitney test was used for the continuous variables with non-parametric distribution and the Wilcoxon test for analyzing the intra-group. Kaplan Meier and Cox regression survival analyses was also used. The chi-square test was applied to compare categorical variables. Furthermore, a binary logistic regression analysis was performed among the groups.
ResultsIn total 188 patients were included in the survey, with 56 patients in 2011, 79 patients in 2012 and 53 patients in 2013, of which 37 patients had VAP, 20 of whom were diagnosed clinically and 17 clinically and microbiologically.
Table 1 shows the statistical comparison of the patients’ clinical characteristics of those with and without VAP. The variables associated with VAP in univariate analysis were use three or more antibiotics prior to infection (p<0.001); enteral nutrition while in the ICU (p<0.01); and tracheostomy (p<0.01). VAP associated mortality rate was 64% (p<0.05) and lastly, the presence of infection represented an additional hospital cost of R$ 7302.70 per day (p<0.01). Through multivariate analysis (Table 2), it was observed that age was an independent factor for VAP (p<0.05; OR 26.99).
Clinical characteristics of patients admitted to a Brazilian hospital on mechanical ventilation from July 2011 to December 2013.
| Variables | VAP (n=37) | No VAP (n=151) | p Value | OR | ||
|---|---|---|---|---|---|---|
| Gender (M/F) | 26 (70.3%) | 11 (29.7%) | 84 (55.6%) | 67 (44.4%) | 0.10 | 0.53 (0.24–1.15) |
| Age, y (≥65, <65) | 23 (62.2%) | 14 (37.8%) | 68 (45.1%) | 83 (54.9%) | 0.06 | 2.0 (0.95–4.19) |
| Antibioticsa | 33 (89.2%) | 46 (30.9%) | <0.01c | 18.83 (6.30–56.23) | ||
| Enteral nutrition | 36 (97.3%) | 77 (51%) | <0.01c | 34.59 (4.62–258.84) | ||
| Tracheostomy | 30 (81.1%) | 31 (20.5%) | <0.01c | 16.59 (6.66–41.32) | ||
| APACHE II | 18.51±10.83 | 16.0±9.9 | 0.2 | – | ||
| APACHE IIb | 36.30±27.18 | 28.23±22.49 | 0.06 | – | ||
| Death | 24 (64%) | 68 (59%) | <0.05c | – | ||
| Daily cost (R$) | 9550.81±6172.21 | 2248.11±607.20 | <0.01c | – | ||
APACHE, Acute Physiological and Chronic Health Evaluation; F, female; M, male; OR odds ratio; VAP, ventilator-associated pneumonia; R$, Brazilian currency.
Logistic regression analysis of the clinical characteristics of patients on mechanical ventilation admitted to a Brazilian hospital from July 2011 to December 2013.
| Variables | VAP (n=37) | No VAP (n=151) | p Value | OR | ||
|---|---|---|---|---|---|---|
| Gender (M/F) | 26 (70.3%) | 11 (29.7%) | 84 (55.6%) | 67 (44.4%) | 0.62 | 0.58 (0.68–5.09) |
| Age, y (≥65, <65) | 23 (62.2%) | 14 (37.8%) | 68 (45.1%) | 83 (54.9%) | 0.05c | 26.99 (1.16–627.33) |
| Antibioticsa | 33 (89.2%) | 46 (30.9%) | 0.16 | 10.21 (0.54–190.73) | ||
| Tracheostomy | 30 (81.1%) | 31 (20.5%) | 0.16 | 33.90 (1.91–601.5) | ||
| APACHE II | 18.51±10.83 | 16.0±9.9 | 0.38 | – | ||
| APACHE IIb | 36.30±27.18 | 28.23±22.49 | 0.93 | – | ||
APACHE, Acute Physiological and Chronic Health Evaluation; F, female; M, male; OR odds ratio; VAP, ventilator-associated pneumonia.
The demographic and clinical characteristics of the group of patients with and without the FAST HUG checklist are shown in Table 3. In univariate analysis, the number of antibiotic-therapy days was significantly higher for those who used three or more antibiotics (p<0.001). Furthermore, by using APACHE II, patients undergoing FAST HUG had more severe clinical conditions at admission (p<0.01), which increased the mortality risk (p<0.05). However, after the implementation of FAST HUG, there was a decreased occurrence of VAP among these patients (p<0.01), as well as a mortality reduction (p<0.01). Additionally, the intervention performed in the study resulted in a significant reduction in ICU hospital costs (p<0.05).
Analysis of demographic and clinical characteristics of patients with and without FAST HUG admitted to a Brazilian hospital from July 2011 to December 2013.
| Variables | No FAST HUG (n=115) | FAST HUG (n=73) | p Value | OR |
|---|---|---|---|---|
| Gender (M/F) | 57/43 | 35/65 | 0.86 | – |
| Age, y (≥65, <65) | 58 (50.4%) | 33 (45%) | 0.80 | – |
| Hospitalization (days) | 16 (8.5–35.5) | 19 (9–47) | 0.32 | 0.99 (0.98–1.0) |
| Antibiotics (days) | 17 (9–140) | 8 (5–57) | <0.001c | – |
| Antibioticsa | 71 (62%) | 25 (34%) | <0.001c | – |
| Surgical | 6 (5%) | 3 (4%) | 0.72 | 0.77 (0.18–3.21) |
| Clinical | 101 (88%) | 66 (90%) | 0.58 | 1.37 (0.5–3.4) |
| Trauma | 9 (8%) | 6 (8%) | 0.92 | 1.05 (0.35–3.09) |
| MV time | 14 (6–140) | 15 (5–139) | 0.16 | 0.99 (0.98–1.0) |
| APACHE II | 14.75±9.8 | 20.22±9.87 | <0.01c | – |
| APACHE IIb | 26±22 | 35±26 | <0.05c | – |
| VAP | 30 (26) | 7 (9,6) | <0.01c | 0.30 (0.12 –0.32) |
| Death | 70 (60) | 22 (30) | <0.01c | 0.27 (0.14–0.51) |
| Daily cost (R$) | 6700.20±26,154.29 | 6339.34±24,529.83 | <0.05c | – |
APACHE, Acute Physiological and Chronic Health Evaluation; F, female; M, male; MV, mechanical ventilation; OR odds ratio; VAP, ventilator-associated pneumonia; R$, the Brazilian currency.
Through logistic regression analysis, significantly less days of antibiotic use (p<0.0001) and a lower mortality rate (p<0.05) could be seen as a result of FAST HUG.
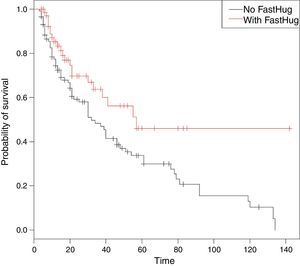
The survival analysis showed that longer length of stay in the ICU was associated lower survival (Fig. 1), and that patients undergoing FAST HUG survived longer. Cox regression was adjusted to the risk factors identified in the logistic regression analysis; antibiotics, enteral nutrition and tracheotomy cases showed events at 38% and censoring 59%, with similarity of the two groups (p>0.05).
However, there was no survival difference between the two groups in the first 20 days of admission. However, considering the first 80 days of hospitalization, 50% of the FAST HUG group survived compared to 20% for those without the intervention. Additionally, as the longer the length of stay, the lower the survival rate for patients without the intervention.
DiscussionVAP is common in patients that are connected to mechanical ventilators over long periods. Therefore, the criteria used for diagnosing VAP is essential.9 Although there are various definitions of VAP, in this study the criteria fever, leucocytosis, chest X-ray with presence with new and progressive pulmonary infiltrates, and microbiological culture are utilized, as these are recommended by the American Thoracic Society3,8; these criteria also present low cost and are commonly used by ICUs for the diagnosis of VAP. On the other hand, these criteria have limitations: there are patients who despite having present VAP symptoms, do not fulfill the more rigorous criteria and would therefore be missed as having VAP.9 VAP is a health care related infection and is the second leading cause of nosocomial infections linked to morbidity and mortality.10 Therefore, the implementation of care guidelines protocols has become necessary for the adequate treatment and care of critically ill patients in ICUs.3,5 An excellent alternative is the creation of checklists. They are simple and easily implemented by multidisciplinary teams working in a hospital.7,11
In order to reach the goals of this study, the authors assumed that a checklist is an indispensable tool for safety and care of critically ill patients. It is suggested that healthcare workers who make bedside rounds adopt a memorization technique of one sentence. This can be associated to a letter to represent the problems that must be evaluated and corrected daily in critically ill patients. Through the expression or acronym FAST HUG, clinical aspects of great importance are highlighted such as nutrition, analgesia, headboard height, and others that characterize prophylactic measures for VAP.7
In relation to the research, various risk factors (the use of more than three antibiotics, enteral nutrition, and tracheotomy) were significantly associated with VAP. The use of antibiotics has been shown in scientific literature to make up to 50% of all prescriptions in the ICU for patients with VAP.12,13 Regarding enteral nutrition, it is well known that a catheter is present in almost all patients with a MV and increasing the PH increases the risk of VAP, a predisposition to gastric colonization, which thus increase the risk of reflux and aspirations pneumonitis.14 Research conducted in 2003 showed that enteral nutrition was an independent risk factor for VAP (p<0.001), as well as tracheostomy (p<0.001).15 Another study showed, through logistic regression analysis, that tracheostomy (p<0.001) was an independent risk factor that can lead to the development of VAP.16
In this study, a statistically significant additional medical cost was seen in patients with VAP. This has been proven by other studies in the United States, which showed that hospital expenses are significantly higher for patients with VAP ($ 104,983), compared to those without VAP ($ 63,689) [p=0.001].17 In 2012, a project was developed with the aim of reducing VAP rates, which resulted in a decline from 9.47 to 1.9 cases per 1000 ventilator days and thus, producing an estimated savings of approximately $1.5 million.18
In addition, the search for improving the quality of care linked to critically ill patients, thus reducing hospital mortality, and the use of hospital quality indicators, which can lead to better care and lower costs, have been targets of major global agencies aimed at preventing diseases and iatrogenesis. Therefore, it is essential to use what has come to be known as packaged measures.14 In applying FAST HUG to critically ill patients daily, resulted in: a decrease in antibiotics use, lower mortality rates, lower hospital costs, and most importantly, it significantly reduced the number of VAP cases. Not to be forgotten that patients diagnosed with a severe illness at hospital admittance have higher mortality risk. Patients who were part of the FAST HUG program were more likely to survive than those without the intervention. A study published in 2008 in an ICU of an American University Medical Center showed a significant reduction of VAP cases after implementing FAST HUG. The rate before FAST HUG implementation was 16.6 cases of VAP per 1000 days of mechanical ventilation, dropped to 1.3 cases after the implementation.19 A multicenter study of ICUs in the United States and Canada between 2002 and 2004 showed significant reduction in VAP, and other more recent studies have shown that implementing FAST HUG caused a 41% reduction rate in VAP.20,21
ConclusionThe implementation of FAST HUG reduced the number of VAP cases, the mortality rate and hospital costs, as well as improved the quality of care. FAST HUG is a package of relatively simple actions that does not overload healthcare professionals, and does not lead to an increase in hospital costs. Its implementation requires nothing more than an administrative decision and personnel preparation and training to bring benefits, particularly to patients. Due to the relative simplicity linked to the program, it can be extended to different public and private institutions without interfering with other plans of action.
Conflicts of interestThe authors declare no conflicts of interest.