While the outbreak has reached every region of the world, it is undeniable that countries in the southern hemisphere seem to be less affected, where cases have been reported, these have been imported and travel related. We analyzed the climate temperature from various regions according to their current ongoing human-to-human transmission status. We studied 3 groups; Group 1, 10 provinces from China with majority of COVID-19 cases; Group 2, areas where continuous horizontal transmission outside of China had been reported; and group 3, areas where imported cases had been detected and no horizontal transmission had been documented after at least seven days since the first case was reported. The regions without ongoing human-to-human transmission showed significantly higher temperatures when compared to China and countries with ongoing human-to-human transmission, with over an 11-degree difference. The average rainfall during the study period was significantly higher in those regions without OHHT when compared to the Chinese provinces with ongoing human-to-human transmission and the regions with active transmission of SARS-CoV-2. Our findings show statistically significant differences between regions with ongoing human-to-human transmission of COVID-19 cases compared to those regions without horizontal transmission. This phenomenon could have implications in the behavior of the ongoing COVID-19 outbreak in the following months.
Currently more than 60 countries have been affected and almost 100,000 cases worldwide have been reported since the beginning of the novel coronavirus infection (COVID-19) outbreak.1 SARS-CoV-2 (taxonomic name of the virus causing COVID-19) has shown diverse disease severity, raging from asymptomatic to acute respiratory disease syndrome with a 1.4–2.3% mortality rate.2,3
While the outbreak has reached every region of the world except Antarctica, it is undeniable that countries in the southern hemisphere seem to be less affected, and were there have been cases reported the majority have been imported and travel related.1 There has been speculation that as temperatures increase with Spring and Summer in the Northern Hemisphere there will be an associated decline in the number of cases. If true, this gives hope to the regions where Spring is starting soon, but also should cause concern in the southern hemisphere were Autumn is to begin.
We sought to analyze the climate temperature from various regions according to their current ongoing human-to-human transmission (OHHT) status. We studied 3 groups; Group 1, 10 provinces from China with majority of COVID-19 cases since December 31, 2019 through February 29, 2020 (92.2% of the total cases in China): Hubei, Guangdong, Henan, Hunan, Shandong, Jiangsu, Sichuan, Hebei, Zhejiang, and Anhui. Group 2, areas where continuous horizontal transmission outside of China had been reported: Italy (Lombardo and Veneto), South Korea (Daegu, Gyeongbuk, Gyeonggi), and Iran (Theran Qom, Gilan); and group 3, areas where imported cases had been detected and no horizontal transmission had been documented after at least seven days since the first case was reported: Philippines (Tagbilaran and Manila), Belgium (Brussels), Findland (Rovaniemi), Egypt (Cairo), and Australia (Melburne, Sidney and Brisbane).
Daily registered maximum and minimal ambient temperatures were obtained from the Weather Channel website (https://weather.com/) from all studied regions, using their biggest metropolitan area as reference. For comparison of mean maximum and minimum temperatures Student T test or Mann–Whitney U test were performed.
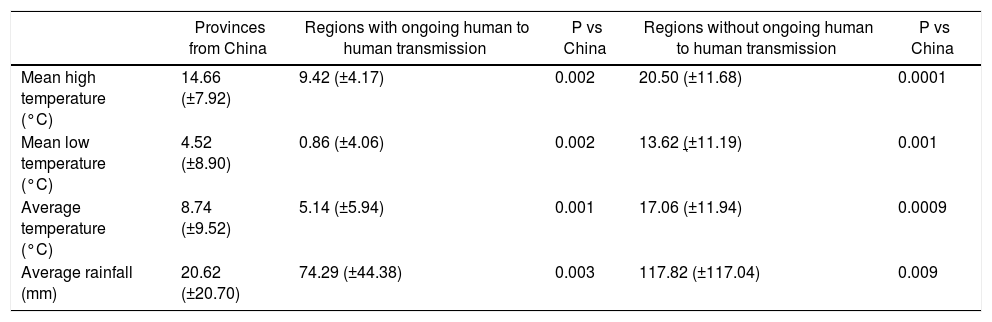
The regions without OHHT showed significantly higher temperatures when compared to China and countries with OHHT, with over a 1°C difference. The regions with OHHT had the lowest temperatures such as China and other regions of group 2. For countries without OHHT the average temperature was 8.32°C higher compared to the other groups (Table 1). The average rainfall during the study period was significantly higher in those regions without OHHT when compared to the Chinese provinces with OHHT (>97.2mm more rainfall) and the regions with active transmission of SARS- CoV-2 (>43.5mm more rainfall).
Comparison of temperature and rainfall among the different regions.
| Provinces from China | Regions with ongoing human to human transmission | P vs China | Regions without ongoing human to human transmission | P vs China | |
|---|---|---|---|---|---|
| Mean high temperature (°C) | 14.66 (±7.92) | 9.42 (±4.17) | 0.002 | 20.50 (±11.68) | 0.0001 |
| Mean low temperature (°C) | 4.52 (±8.90) | 0.86 (±4.06) | 0.002 | 13.62 (±11.19) | 0.001 |
| Average temperature (°C) | 8.74 (±9.52) | 5.14 (±5.94) | 0.001 | 17.06 (±11.94) | 0.0009 |
| Average rainfall (mm) | 20.62 (±20.70) | 74.29 (±44.38) | 0.003 | 117.82 (±117.04) | 0.009 |
It has been described that temperatures and environmental factors contribute to the survival of different coronavirus.4 Studies have found that low temperatures and dry conditions favor MERS-CoV survival and dissemination; nevertheless, Altamimi et al.5 found that high temperatures, coupled with high ultraviolet index, low wind speeds, and low relative humidity were contributors to increased MERS-CoV cases.
Slight differences in temperature have a significant impact on MERS CoV and SARS CoV survival in the environment. Otter et al.6 compiled various studies addressing the survival of respiratory viruses on surfaces and showed that slight differences in temperature and relative humidity reduce or enhance viability; some of these variations were similar to those found in our analysis.
Although temperature and humidity changes in the environment can potentially affect the behavior of SARS-CoV-2 in a community. These are factors that can be easily adjusted in the hospital setting, so that some of the extremes in temperature and relative humidity may not apply in the hospital.
To further complicate the analysis, environmental climate changes may not favor respiratory virus pandemics as expected, the initial cases of influenza A H1N1 2009 started at the end of the regular influenza season in Mexico (March–April 2009) and went on to have an enormous impact during the following summer months.7
Our selection criteria for the regions tried to compensate the variations that many countries have in detection practices and resources for this purpose as well as the possibility of under reporting that may limit the extent our findings. In conclusion, there were statistically significant differences among regions with OHHT of COVID-19 cases compared to those regions without horizontal transmission. This phenomenon could have implications in the behavior of the ongoing COVID-19 outbreak in the following months.
Conflicts of interestThe authors declare no conflicts of interest.