Human cytomegalovirus (CMV) is the most common cause of congenital infection, with morbidity and mortality at birth.1–5 Usually, there are no clinical symptoms for CMV during primary infection, reactivation, and re-infection with a different CMV strain, but infected individuals may transmit the virus via body fluids such as saliva, blood, cervical secretion, semen, and urine.1–4 The risk of intrauterine infection largely depends on the time of maternal infection during pregnancy – it is lowest at the time of conception, and is increased in the third trimester.4 Some studies concluded that CMV infection lead to miscarriage and stillbirth.4,5
The need for diagnostic tests at all stages of gestation has always been the subject of debate due to the insufficient evidence of congenital abnormalities in re-infection. Thus, the CMV infection diagnostic test is still not considered part of routine prenatal tests.4,5 Currently, no national screening test for CMV infection is available at all stages of pregnancy in Iran.
Considering the importance of intrauterine CMV infection transmission and its complications, it is necessary to study the prevalence of CMV infection in pregnancy with regional interests. The aim of this study was to determine the seroprevalence of CMV infection in a pregnant population in Eastern Iran. The effects of age, residency, abortion, parity, and education on the seroprevalence of the infection have also been investigated.
In this descriptive study, 240 serum samples were collected from pregnant women at the third trimester from February to April, 2011, using the ELISA method, to measure CMV IgG and IgM markers. The IgG avidity test was used for all patients who were CMV-IgM+ and CMV-IgG+ to distinguish between primary and recurrent CMV infection. All CMV-IgM+ of pregnant women were monitored until labor.
This study was approved by the Ethical Review Committee of the Islamic Azad University, Gonabad Branch, Gonabad, Iran.
In our study, the CMV seroprevalence rate was 72.1%. Among the 240 tested women, 167 (69.6%) had had a previous CMV infection and 67 (27.9%) had never been infected with CMV. The remaining six (2.5%) women were CMV-IgM+. In the latter group, four women (1.66%) had recurrent CMV infection (IgM+ and high IgG avidity) and two (0.84%) women had primary CMV infection (IgM+ and low IgG avidity).
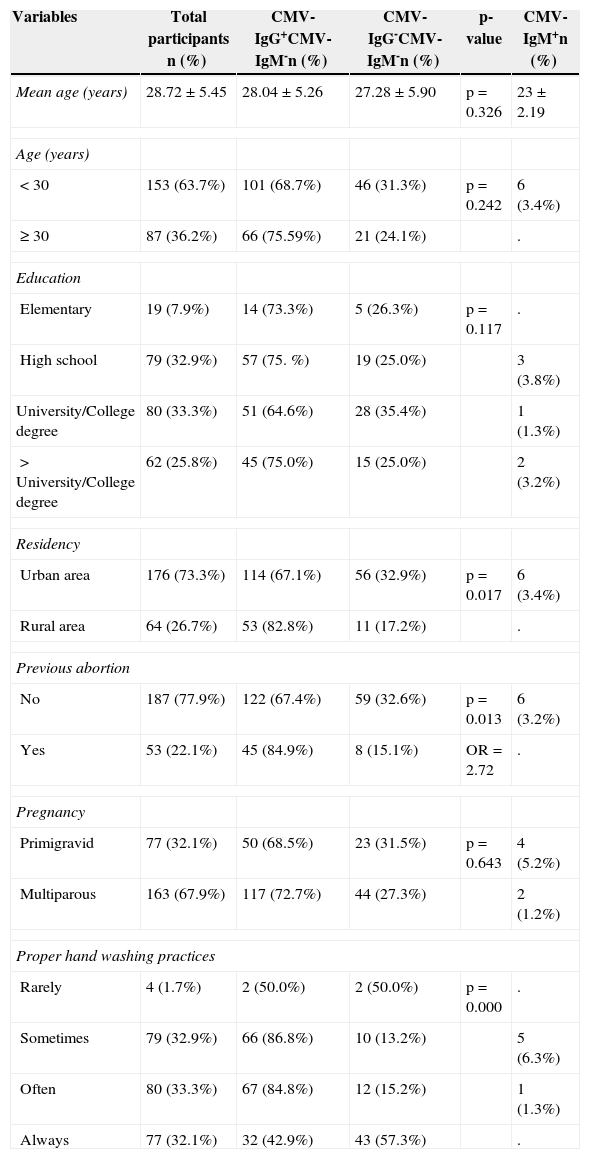
There was significant correlation of history of abortion, residence place, and personal hygiene status with IgG seropositivity rate (Table 1). Two CMV-IgM+ subjects were faced with preterm labor and low birth weight. Due to the small number of CMV-IgM+ pregnant women, we could not draw any definitive conclusion about the consequences to pregnancy. Further studies should follow-up women with primary and recurrent CMV infection in the third trimester of pregnancy.
Distribution of CMV seroprevalence regarding the studied variables.
| Variables | Total participants n (%) | CMV-IgG+CMV-IgM-n (%) | CMV-IgG-CMV-IgM-n (%) | p-value | CMV-IgM+n (%) |
|---|---|---|---|---|---|
| Mean age (years) | 28.72±5.45 | 28.04±5.26 | 27.28±5.90 | p=0.326 | 23±2.19 |
| Age (years) | |||||
| <30 | 153 (63.7%) | 101 (68.7%) | 46 (31.3%) | p=0.242 | 6 (3.4%) |
| ≥ 30 | 87 (36.2%) | 66 (75.59%) | 21 (24.1%) | . | |
| Education | |||||
| Elementary | 19 (7.9%) | 14 (73.3%) | 5 (26.3%) | p=0.117 | . |
| High school | 79 (32.9%) | 57 (75. %) | 19 (25.0%) | 3 (3.8%) | |
| University/College degree | 80 (33.3%) | 51 (64.6%) | 28 (35.4%) | 1 (1.3%) | |
| >University/College degree | 62 (25.8%) | 45 (75.0%) | 15 (25.0%) | 2 (3.2%) | |
| Residency | |||||
| Urban area | 176 (73.3%) | 114 (67.1%) | 56 (32.9%) | p=0.017 | 6 (3.4%) |
| Rural area | 64 (26.7%) | 53 (82.8%) | 11 (17.2%) | . | |
| Previous abortion | |||||
| No | 187 (77.9%) | 122 (67.4%) | 59 (32.6%) | p=0.013 | 6 (3.2%) |
| Yes | 53 (22.1%) | 45 (84.9%) | 8 (15.1%) | OR=2.72 | . |
| Pregnancy | |||||
| Primigravid | 77 (32.1%) | 50 (68.5%) | 23 (31.5%) | p=0.643 | 4 (5.2%) |
| Multiparous | 163 (67.9%) | 117 (72.7%) | 44 (27.3%) | 2 (1.2%) | |
| Proper hand washing practices | |||||
| Rarely | 4 (1.7%) | 2 (50.0%) | 2 (50.0%) | p=0.000 | . |
| Sometimes | 79 (32.9%) | 66 (86.8%) | 10 (13.2%) | 5 (6.3%) | |
| Often | 80 (33.3%) | 67 (84.8%) | 12 (15.2%) | 1 (1.3%) | |
| Always | 77 (32.1%) | 32 (42.9%) | 43 (57.3%) | . | |
Failure to detect asymptomatic infected neonates, who are at the risk of complications such as sensorineural hearing loss, vision loss, and mental retardation, can have a negative effect on the development of children.2,4 The application of a noninvasive serological assay to detect CMV infection would be advantageous for asymptomatic newborns, though it could not change the outcomes of pregnancy.
Conflict of interestAll authors declare to have no conflict of interest.